D Bozec1, M P Robinson2 and C A Marshman1
1. York EMC Services Ltd, The University of York, Heslington, York YO10 5DD
Principal contact: This email address is being protected from spambots. You need JavaScript enabled to view it.
2. Department of Electronics, The University of York, Heslington, York YO10 5DD
ABSTRACT
Electromagnetic compatibility (EMC) - the ability of electronic systems and devices to function well in close proximity to each other - has traditionally been given scant attention in the design and construction of healthcare facilities. Hospitals contain some types of equipment, such as electrosurgery units and short-wave diathermy applicators, that are known to produce high levels of electromagnetic interference (EMI), and other types such as ECG (Electrocardiography) and EEG (Electroencephalography), which are known to be particularly sensitive to electromagnetic disturbances. Despite the existence of standards and regulations, there is often no collaboration between the designers of the buildings and the users of the equipment therein. In this paper, we show how an understanding of EMC enables us to prevent interference problems and protect critical systems. We discuss how good installation and maintenance practices such as the use of zoning and safe distances can ensure that adequate levels of EMC are achieved in the hospital environment.
1. INTRODUCTION
Is electromagnetic compatibility (EMC) of medical equipment a problem in the healthcare environment? Although electrical interference in hospitals is often regarded as no more than a minor nuisance, there are documented cases in which equipment failures due to electromagnetic interference (EMI) have lead to injury or death. Some examples follow:
- In 1992, a patient attached to a monitor-defibrillator in an ambulance died because interference from the ambulance radio prevented the machine from working (1).
- In 1987, patient monitoring systems failed to sound alarms because of interference; two patients died as a result (2).
- In 1993, a patient fitted with a pacemaker went into ventricular fibrillation shortly after being scanned with a metal detector outside a courtroom (2).
As in many other fields, the amount and complexity of electronics in hospitals and other medical environments is increasing year by year. Despite this, the number of reported incidents of EMC problems fortunately does not appear to be growing. This is probably because most manufacturers and designers of medical electronic products have developed a good awareness of EMC. Pacemakers are typical examples, where their design with respect to compactness and immunity to radio frequency interference has greatly improved over the years. Nowadays, pacemakers are very reliable, but can still fail under extreme conditions. Pacemakers have failed in patients undergoing electrosurgery (2) (not surprisingly as this is not recommended) and in other cases where patients kept mobile phones in their chest pockets, a few centimetres from the subcutaneous pacemaker leads (3). The powered wheelchair is another typical example: there are many stories of radiofrequency interference (RFI) from mobile phones or police 'walkie-talkies' causing the wheelchair to drive itself and its occupant into traffic or a cliff. These stories are based on real occurrences; reports of incidents in the USA in the early 1990s prompted the Food and Drug Administration (FDA) to investigate the problem and recommend that the manufacturer change the design to give an immunity of at least 20V/m to RFI.
With respect to the legislation in place, electro-medical equipment carries the CE marking demonstrating that it conforms to either the Medical Devices Directive (MDD) (4), the Active Implantable Medical Devices Directive (AIMD) (5) or the In Vitro Diagnostic Medical Directive (6). The conformance is in most cases demonstrated by meeting the requirements of EN 60601-1-2 (7) or EN 55011 (8) in the case of Industrial, Scientific and Medical (ISM) equipment. Other electronic/electrical equipment such as Information Technology Equipment (ITE) will carry the CE marking to show that it meets the requirement of the EMC Directive 89/336/EEC. However it is necessary to inspect the Declaration of Conformity (DoC) to identify if the equipment has been tested to the relevant standards specific to the environment before the equipment is put into service. The use of many items of electronic equipment in the hospital environment, such as therapeutic equipment (equipment intentionally designed to emit electromagnetic energy) and diagnostic equipment such as electrocardiography (ECG) requires some electromagnetic (EM) management and formal planning to ensure that the potential for interference and therefore for potential EM hazard is minimised (9).
EMC should also be an integral part of the design process when planning for the construction of healthcare facilities: the electrical distribution of hospitals can be quite varied and complex and it is important to ensure that the distribution does not provide a means to propagate EMI throughout the building. For instance, community hospitals are currently being built in the United Kingdom, where the electrical distributions are installed using simple twin-and-earth cables, quite often running parallel and in very close proximity to hospital data network. The use of twin-and-earth cable does not provide any protection of EMI (as no shielding is provided), and therefore it is extremely likely that crosstalk (unintentional coupling of electrical energy from one cable to another) will occur. Standards, such as EN 50147-2:2001 (10) provide guidelines to achieve good EMC practice to reduce any possibility of EMI problems.
The use of many items of electronics equipment in close proximity in the hospital environment means that the same sort of EMC problems are encountered as with other types of electronic products. However there are some special features of the hospital EM environment:
- Failure of medical devices can lead to injury or death
- In the European Union, medical products are not covered by the EMC Directive but by the three product-specific directives.
- Some equipment found in hospitals is intentionally designed to emit electromagnetic energy, often for therapy. Other equipment, which may be located nearby, is designed to detect very small physiological signals. This combination has the potential to create EMC problems.
- Also in hospitals, there is the question of whether to ban or restrict the use of mobile phones. They improve communications but can interfere with critical equipment.
- Many medical devices are connected directly to patients. For mains-powered devices, the designer must prevent electric shock as well as ensure EMC.
Electronic equipment is constantly evolving, so there is always the possibility of new problems arising, e.g. interference from new types of mobile communications devices (such as UMTS, 3G, wireless LANs and TETRA). It is the responsibility of many people to prevent EMC problems from endangering patients:
- Manufacturers and designers of equipment can ensure that equipment meets appropriate emissions limits and levels of immunity.
- Hospital administrators, planners and architects can keep potential sources and victims of EMI apart.
- Users should be aware of the threat of EMI and should also be encouraged to report any serious incidents.
2. EMC LEGISLATION AND STANDARDS IN EUROPE
Before 1993, each European country had its own system of regulating the manufacture and sale of medical equipment. In order to unify legislation, the European Union has been introducing a series of directives, thus removing barriers to trade and promoting the Single Market.
2.1 The medical devices directive
Most electronic equipment is covered by EMC Directive 89/336/EEC. However medical equipment is covered by one of three product-specific directives:
- The Medical Devices Directive (MDD) 93/42/EEC; in force since 1998 (4).
- The Active Implantable Medical Devices Directive (AIMD) 90/385/EEC: in force since 1995 (5).
- The In Vitro Diagnostic Directive (IVDD) 98/79/EC: in force since 1998 (6).
Most medical equipment must comply with the MDD to be allowed to carry the CE Marking. Each member state is required to appoint a Competent Authority to implement and enforce the MDD. In the UK this is the Medical Devices Agency (MDA). The Competent Authority appoints Notified Bodies to administer conformity.
The Medical Devices Directive became fully implemented by UK regulations on 13 June 1998 at the end of a transitional period. For electromedical products, this means that they must comply with electrical safety requirements as well as other requirements of the MDD. In common with other new approach directives this compliance may be demonstrated by conforming to the requirements of standards whose reference numbers have been published in the Official Journal of the European Community (OJEC). For electromedical devices the relevant standard is EN60601-1, which is the CENELEC adoption of IEC 601-1. Part 2 of EN60601-1 specifies EMC requirements (7).
2.2 Standard EN60601-1-2
This standard applies to medical electrical equipment, medical electrical systems, information technology equipment used in medical applications and all other equipment forming part of medical electrical systems.
In common with modern EMC standards, EN60601-1-2 defines limits for emissions and levels of immunity. To assess apparatus to these limits and levels, test methods are defined by making reference to 'basic' standards. In this case the basic standards are:
- CISPR 11 (the product specific standard for Industrial, Scientific and Medical, ISM, equipment) for emissions (8).
- EN 61000-4 series immunity standards (9).
Following many years of discussion the standard was recently updated to encompass the frequencies used by mobile phones and other communications technologies such as wireless local area networks (WLANs). It is worth noting that standards such as EN60601-1-2 specify levels of EMC performance but do not tell designers and installers of devices and systems how to go about achieving compliance.
3. Medical Electromagnetic Environments and EMI
3.1 General nature of EMI
The world's industrialised nations are becoming increasingly dependent upon the use of electrical and electronic equipment. Whether it is in the home, or in industry and commerce, everybody is being affected by this trend. As our society becomes increasingly dependent upon electrical/electronic systems of different types for its day-to-day activities, the number and diversity of EMI sources can also be expected to increase; the corresponding effects of EMI are likely to become more varied, and possibly more subtle. These effects cause particular concern if they form a direct threat to public health and safety, or if they cause key electrical/electronic systems to malfunction, e.g. in healthcare facilities, manufacturing industry, communications or defence. Additionally, if the levels of EMI exceed specified limits, without necessarily giving rise to malfunctions, this is also a cause for concern since it will provide an EMI environment which is more severe than that assumed in specifications and standards; new equipment and systems subsequently introduced into that environment thus have a higher probability of malfunctioning.
In general, EMI sources affecting a particular electrical or electronic system can be classified under the two headings of 'internal' EMI and 'external' EMI. Internal EMI is associated with the devices and components which are present within the system, e.g. resistors, transistors etc.
External EMI is generated by sources outside the system in question. Typical sources could be car ignition systems, fluorescent lighting, electrical motors or generators, microcomputers, thunderstorms, solar disturbances, etc.
It is external EMI that is normally of greatest significance in the EMC context. However, internal noise may place a fundamental limitation on measurement precision. In the remainder of this paper, attention will be confined to external sources of EMI.
The effects of EMI are a cause of great concern to designers, manufacturers, importers, retailers and users of electrical and electronic equipment. Such equipment must be designed to operate satisfactorily in the environment for which it is intended, and without affecting existing equipment. In other words equipment must be designed to have in-built compatibility.
3.2 EMI propagation mechanisms
For electromagnetic disturbances to cause interference, they must be propagated in some way. The three main physical mechanisms of electromagnetic propagation are:
- Conduction
- Reactive coupling
- Radiation.
 Fig 1: Schematic description of EMI coupling paths (adapted from (12))
Fig 1: Schematic description of EMI coupling paths (adapted from (12))
3.2.1 Conduction
Electromagnetic energy may be conducted in either common mode or differential mode. This can be via power cables, earth conductors, signal cables, antenna feeders or other low impedance paths. There is greater risk from conducted interference at frequencies below 30 MHz. Above this frequency conducted interference suffers substantial attenuation and other propagation mechanisms become dominant.
In a hospital, EMI can often be propagated via the mains distribution network (20). As was noted above, the type of cables used and the way they are laid out can have a big effect on levels of conducted interference.
3.2.2 Reactive coupling
Electromagnetic energy may also be propagated by reactive coupling, either inductive or capacitive. The precise effects depend upon distance, orientation, size, earthing and other factors all of which will tend to be unique to the system. Reactive coupling may exist within a system, or between systems.
In general, inductive coupling tends to be associated with high current and low impedance situations, whilst capacitive coupling tends to occur with high voltages and high impedance. Often both types are present together. Reactive coupling between wires is called crosstalk, and often occurs when different types of cables are bundled together over long distances.
3.2.3 Radiation
For frequencies above about 30 MHz, radiation tends to be the dominant propagation mechanism. There are two types of radiating emitters: intentional and unintentional. Intentional emitters, such as radio and radar, produce spurious emissions together with their intended signal. These may be in the form of harmonics or inter-modulation products of the intended signal and are directly associated with the primary function of the equipment. Practical radio transmitters also radiate broadband noise. Unintentional emitters, for example personal computers or thyristor drives, generate emissions as a by-product of the primary function of the equipment.
A useful measure of radiated emissions is the electric field strength, generally expressed in volts per metre, V/m. Surveys of the EM environment in hospitals tend to find that the field strength from external transmitters (such as radio and TV masts) is less than 1V/m. The standard EN60601-1 specifies an immunity to RFI of up to 3V/m for most devices, and 10V/m for safety-critical equipment.
It should be noted that, in any given situation, EMI propagation may well be via a combination of two or three of the above mechanisms, rather than being due to a single mechanism in isolation.
3.3 Sources of EMI
Typical sources in hospitals include motors, fluorescent lights, switch-gear and equipment fitted with switched mode power supplies.
Electrosurgery, also known as electrocautery or surgical diathermy, is a great source of EMI in hospitals (13). Currents of over 1A and EMFs of over 4kV are used to cut and coagulate tissue. A typical frequency is 500kHz, which is high enough not to give the patient electric shocks. However it also means that the equipment radiates at harmonics of this frequency, especially between 1 and 10MHz. This type of equipment is so good at creating EMI that it was adapted during the Second World War for jamming radar. It can generate fields of 40-50V/m at 1m (14), making it difficult to use monitors in the same room. Pacemakers can also be affected. Shielding is not feasible because the patient forms part of the radiating antenna. However problems can be reduced by careful placement of leads.
SW Physiotherapy operates at the ISM frequency of 27MHz (15). It deposits energy to warm tissue. The RF signal is usually pulsed, although there is little evidence that this is clinically beneficial. This creates problems through demodulation giving an audio signal, giving buzzing noises on telephones. Computing, monitoring and video equipment nearby can be disrupted. Better shielding of applicators reduces the problem.
Another source of EMI is mobile radio transmitters - cellular phones and emergency services radios. These generate very high field strengths but only at short distances. Theoretically the field varies inversely with the distance from the antenna, and can be estimated using the expression 7√ P / d where P is the radiated power in watts and d is the distance in metres. However there is some evidence that hospital corridors have a 'guiding' effect on the radiation and that the fields fall off slightly more slowly than this. A number of studies in the 1990s (e.g. (16),(3)) showed that a wide range of equipment can be susceptible to RFI from mobile radio transmitters. Fortunately, EMI from cellular phones is unlikely at distances of greater than 2m. High field strengths are produced not only by handsets but also by the transmitters on ambulances and other emergency vehicles (17).
3.4 Victims of EMI
Any piece of equipment will fail if subjected to a large enough disturbances. Digital circuits are generally more immune but fail more catastrophically when they eventually do so. Circuit failure is not necessarily hazardous to patients. A wobbly picture on a monitor would probably be regarded as no more than a nuisance, whereas failure of a ventilator, infusion pump or automated defibrillator could be fatal.
Devices designed to pick up electric or magnetic fields are obviously vulnerable. An example is a hearing aid fitted with a telecoil option or 'T-switch' (18). This enables the aid to pick up magnetic fields from telephones, and also from specially fitted induction loops in meeting halls, churches etc. Unfortunately this system is susceptible to low frequency radiation fields from motor drives, telecommunications cables and computer monitors, which are not covered by EMC standards because they are below 150kHz.
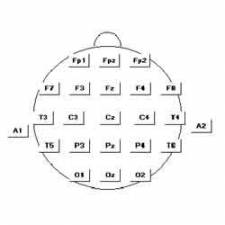
Physiological-monitoring equipment is vulnerable to pulsed RF, which can be demodulated by non-linear elements in amplifier circuits. Some monitors are connected directly to the patient in order to detect small physiological signals, as shown in the following table:
| Measurement | Typical voltage |
| Electrocardiography (ECG) | 1mV |
| Electroencephalography (EEG) | 100µV |
| Electromyography (EMG) | 10µV |
| Evoked potentials | 1µV |
EEG is known to be very sensitive to EMI. External pacemakers incorporate ECG sensors and have been shown to be vulnerable to the 17Hz pulse rate of the TETRA system for private radio, which is currently being taken up by the police and other emergency services (19).
Mains-powered equipment, including ventilators, anaesthesia machines and syringe pumps, can also be vulnerable to conducted interference on the mains supply. Battery/mains equipment, which runs on a battery with continuous charging from the mains has very good immunity to mains voltage variations such as drop-outs and sags (20).
4. CONCLUSION
EMC is a concern not just for manufacturers, but also for those who install, use, modify or maintain medical equipment. The existence of directives and standards has encouraged good EMC design practices, but should not be relied on to prevent EMI problems owing to the nature of the hospital EM environment. Much can be done by promoting awareness of EMI and its underlying coupling mechanisms. Many potential problems can be resolved by ensuring adequate separation of sources and victims of interference: for example by placing SW diathermy or electrosurgery in a different part of the building to EEG and other sensitive equipment, by implementing sensible restrictions on mobile phones, by considering the radiation from the vehicles' antennas when choosing a location for ambulance bays, and by avoiding crosstalk problems when installing mains and data cables.
REFERENCES
(1) 'Banana Skins', UK EMC Journal, vol. 15, p. 8, February 1998.
(2) Jeffrey L Silberberg, 'Performance degradation of electronic medical devices due to electromagnetic interference', Compliance Engineering vol. 10 p. 25 1993.
(3) Medical Devices Agency, 'Electromagnetic Compatibility of Medical Devices with Mobile Communications', MDA DB 9702, 1997.
(4) The EC Medical Directive 93/42/EEC - Official Journal L169-1993.
(5) The EC Active Implantable Medical Directive 90/385/EEC - Official Journal L189-1990.
(6) The In Vitro Diagnostic Medical Devices Directive 98/79/EC - Official Journal L331-1998.
(7) EN60601-1-2:2001 - Medical Equipment Part 1-2: General requirements for safety Collateral standard: Electromagnetic compatibility - Requirements and tests.
(8) EN55011 1998 (+ Amendment A2:2002) - Industrial, scientific and medical (ISM) radio frequency equipment - Radio disturbance - Characteristics - Limits and methods of measurement.
(9) Christopher Marshman, 'EMC Management and Planning in the Hospital Environment to minimise Hazards' IPEM Conference on 'Practical Methods for Mitigation of EMI and EMF Hazards within Hospitals' 28th January 2003.
(10) EN50174-2:2001 - Information technology - Cabling Installation - Part 2: Installation planning and practices inside buildings.
(11) IEC 801 series standards (EN 61000-4-2, EN 61000-4-3, EN61000-4-4, EN61000-4-5, EN61000-4-6, EN61000-4-8 and EN61000-4-11).
(12)Tim Williams, EMC for Product Designers (Second Edition), Newnes, Oxford, ISBN 0 7506 2466 3. (13) J Gardner, 'Practical problems of electrosurgery', IEE Colloq. on 'Electromagnetic interference in hospitals', Digest no. 1994/190, sec. 6, 1994.
(14) Robert Nelson and Hualiang Ji, 'Electric field strengths created by electrosurgical units', IEEE Int. Symp. EMC, p. 366, 1994.
(15) D Wilton, 'How Physiotherapy generates problems', IEE Colloq. on 'Electromagnetic interference in hospitals', Digest no. 1994/190, sec. 7, 1994.
(16) M P Robinson, I D Flintoft and A C Marvin 1997. 'Interference to medical equipment from mobile phones' J. Med. Eng. Technol. 21 pp 141-146
(17) Medical Devices Agency, 'Emergency service radios and mobile data terminals: compatibility problems with medical devices', MDA DB1999(02), 1999.
(18) Robert Higginson, 'Are you hearing me? An aid for the disabled lacking EMC protection', UK EMC Journal p. 14, June 1998.
(19) I D Flintoft, M P Robinson, S J Porter and A C Marvin 2000. 'Addressing the risks of EMC problems with mobile radio transmitters' Compliance Eng. 17, Sept./Oct. pp 30-38.
(20) R Railton, G D Currie, G A Corner and A L Evans, 'Malfunction of medical equipment as a result of mains borne interference', 8th Int. Conf. EMC, Edinburgh