Electromyography (EMG) is an electro-diagnostic medicine technique for evaluating and recording the electrical activity produced by skeletal muscles. The EMG is performed using an instrument called an electromyograph to produce a record called an electromyogram. An electromyograph detects the electrical nerve signals (potentials) generated by muscle cells when these cells are electrically or neurologically activated. The signals can be analyzed to detect medical abnormalities, activation level, or recruitment order, or to analyze the biomechanics of human or animal movement.
Electromyography (EMG) is an electro-diagnostic medicine technique for evaluating and recording the electrical activity produced by skeletal muscles. The EMG is performed using an instrument called an electromyograph to produce a record called an electromyogram. An electromyograph detects the electrical nerve signals (potentials) generated by muscle cells when these cells are electrically or neurologically activated. The signals can be analyzed to detect medical abnormalities, activation level, or recruitment order, or to analyze the biomechanics of human or animal movement.
The action of nerves and muscle is essentially electrical. Information is transmitted along nerves as a series of electrical discharges carrying information in a pulse repetition frequency. This may be in the range of 1 to 100 pulses per second. Electromyography contraction of muscle fibres is also associated with an electrical discharge which can be detected by measuring electrodes or brought about by electrical stimulation.
EMG is most often used when people have symptoms of weakness, and examination shows impaired muscle strength. It can help to differentiate primary muscle conditions from muscle weakness caused by neurological disorders. EMG can be used to differentiate between true weakness and reduced use because of pain or lack of motivation.
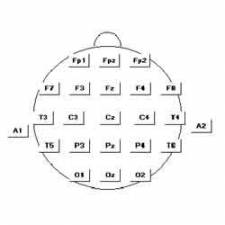
 EMG equipment consists of recording electrodes, preamplifiers (which are normally placed very close to the patient to avoid pick-up of electrical interference), amplifiers to provide the correct gain, calibration and frequency characteristics, a display system (usually a CRT), a range of integrators and averagers - partly to achieve some data compression (chart records may be very long and difficult to read), and a recording medium, which is often a photographic (fibre-optic) system.
EMG equipment consists of recording electrodes, preamplifiers (which are normally placed very close to the patient to avoid pick-up of electrical interference), amplifiers to provide the correct gain, calibration and frequency characteristics, a display system (usually a CRT), a range of integrators and averagers - partly to achieve some data compression (chart records may be very long and difficult to read), and a recording medium, which is often a photographic (fibre-optic) system.
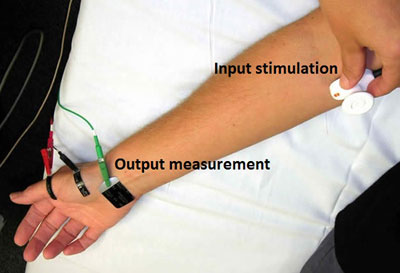
The most typical method for testing uses an electrode stuck to the skin above the muscle. The electrical activity detected by this electrode is displayed on the monitor (and may also be heard audibly through a speaker). Because skeletal muscles are isolated and often large units, each electrode gives only an average picture of the activity of the selected muscle. Several electrodes may need to be placed at various locations to obtain an accurate study. After placement of the electrode(s), the patient may be asked to contract the muscle (for example, by bending the arm).
The presence, size, and shape of the wave form produced (the Action Potential) provides information about the ability of the muscle to respond to nerve stimulation. Each muscle fibre that contracts will produce an action potential (AP); the size of the muscle fibre affects the AP rate (how frequently an action potential occurs) and size (amplitude) of the action potential(s). A nerve conduction velocity test is often done at the same time as an EMG.
 Muscle tissue is normally electrically silent at rest. Once stimulated, action potentials begin to appear on the monitor. As a contraction is increased, more and more muscle fibres produce action potentials until a disorderly group of action potentials of varying rates and amplitudes (complete recruitment and interference pattern) appears with full contraction.
Muscle tissue is normally electrically silent at rest. Once stimulated, action potentials begin to appear on the monitor. As a contraction is increased, more and more muscle fibres produce action potentials until a disorderly group of action potentials of varying rates and amplitudes (complete recruitment and interference pattern) appears with full contraction.
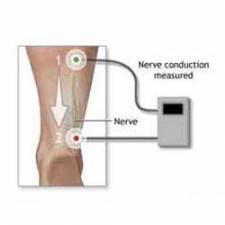
Many EMG tests involve the use of stimulators to induce discharges in a nerve trunk, and detect the response by surface electrodes over a muscle served by that nerve. In this case the signals may be as large as 2 mV, and may be presented audibly or for recording on an electronic chart recorder. Such evoked response tests might be for determining the nerve conduction time, or for assessing the performance of the neuromuscular control system. There are many different disorders of the nervous system and EMG examination has to be tailored to the particular requirements of the individual patient. Thus, these tests are normally carried out by a specialist in electromyography within the neurology department.
Disorders or conditions that cause abnormal EMG results include:
- Polymyositis
- Denervation (reduced nervous stimulation)
- Carpal tunnel syndrome
- ALS
- Myopathy (muscle degeneration, may be caused by a number of disorders, including muscular dystrophy)
- Myasthenia gravis
- Alcoholic neuropathy
- Axillary nerve dysfunction
- Becker's muscular dystrophy
- Brachial plexopathy
- Cervical spondylosis
- Common peroneal nerve dysfunction
- Dermatomyositis
- Distal median nerve dysfunction
- Duchenne's muscular dystrophy
- Facioscapulohumeral muscular dystrophy (Landouzy-Dejerine)
- Familial periodic paralysis
- Femoral nerve dysfunction
- Friedreich's ataxia
- Guillain-Barre
- Lambert-Eaton Syndrome
- Mononeuritis multiplex
- Mononeuropathy
- Peripheral neuropathy
- Radial nerve dysfunction
- Sciatic nerve dysfunction
- Sensorimotor polyneuropathy
- Shy-Drager syndrome
- Thyrotoxic periodic paralysis
- Tibial nerve dysfunction
A nerve conduction study (NCS)
NCS is a measurement of the amount and speed of conduction of an electrical impulse through a nerve. NCS can determine nerve damage and destruction, and is often performed at the same time as EMG. Both procedures help to detect the presence, location, and extent of diseases that damage the nerves and muscles.
Sources:
https://www.hopkinsmedicine.org/healthlibrary/test_procedures/neurological/electromyography_92,p07656
http://www.uhs.nhs.uk/OurServices/Brainspineandneuromuscular/Clinicalneurophysiology/Electromyography.aspx
https://en.wikipedia.org/wiki/Electromyography
https://www.guysandstthomas.nhs.uk/.../neurophysiology-and-epilepsies/specialties/emg/overview.aspx
Edited by John Sandham