What is malnutrition?
 Malnutrition occurs when insufficient food has been eaten so that the body starts to use up its own reserves of energy and protein. Your reserves of sugar, fat and protein become depleted. This leads eventually to potentially severe consequences. You may think of malnutrition as something that occurs in so called developing or third world countries, particularly in Africa or India. It is true that malnutrition is quite common in those areas but it is also surprisingly common in the UK. Up to 40% of those admitted to hospital in the UK already show evidence of malnutrition. The reasons for finding malnutrition in the UK do not relate to shortages of food but to the effect of underlying illnesses, and/or poverty and social deprivation. Malnutrition actually costs the UK more each year than obesity. It has been calculated that up to 3 million people are suffering from malnutrition in the UK. There are many disease processes which are associated with deteriorating nutrition. For example: chronic chest diseases, heart failure, kidney and liver failure and numerous abdominal causes, strokes and other disorders of the nervous system.
Malnutrition occurs when insufficient food has been eaten so that the body starts to use up its own reserves of energy and protein. Your reserves of sugar, fat and protein become depleted. This leads eventually to potentially severe consequences. You may think of malnutrition as something that occurs in so called developing or third world countries, particularly in Africa or India. It is true that malnutrition is quite common in those areas but it is also surprisingly common in the UK. Up to 40% of those admitted to hospital in the UK already show evidence of malnutrition. The reasons for finding malnutrition in the UK do not relate to shortages of food but to the effect of underlying illnesses, and/or poverty and social deprivation. Malnutrition actually costs the UK more each year than obesity. It has been calculated that up to 3 million people are suffering from malnutrition in the UK. There are many disease processes which are associated with deteriorating nutrition. For example: chronic chest diseases, heart failure, kidney and liver failure and numerous abdominal causes, strokes and other disorders of the nervous system.
Good nutrition is important to everyone but crucial to those with disease-related malnutrition or recovering from surgery. The body will then be working extra hard to restore good health, thus increasing nutritional needs.
The nutrients needed to build body tissue and provide energy for bodily functions include: carbohydrates, protein, fat, vitamins, minerals and water.
Normally these are provided by a balanced diet as a result of everyday eating and drinking. However, if a patient has a problem with their digestive system, it may be necessary for them to receive their nutrition in liquid form through a tube. This liquid nutrition is normally delivered by a medical grade Enteral feeding pump.
The two types of artificial nutrition:
- Enteral Nutrition
- Total Parenteral Nutrition
Enteral Nutrition (EN) is received via a fine tube that is placed in one of three ways.
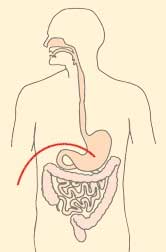
Naso-gastric feeding (NG)
The naso-gastric feeding tube is inserted through the nose and is advanced until it reaches the stomach. Different-sized tubes may be used. In certain cases the tube can be passed down the nose and advanced into the small bowel: this is called a naso-jejunum (NJ) tube.
There are various ways of administering the feed:
- Bolus administers the feed solution over a 15-20 minute period several times a day; Intermittent gravity drip administers the feed solution over 30-60 minutes several times a day;
- Continuous administers the feed solution over a period of between 8-24 hours.
 These methods may be used in combination and will involve the use of an enteral feeding pump or gravity drip.
These methods may be used in combination and will involve the use of an enteral feeding pump or gravity drip.
Each episode of delivery is tailored to individual needs.
Using a 'clean procedure' the tube is connected to the bag of feed solution. The feed is then either pumped in or dripped by gravity.
Due to the potential for displacement of the internal end of Nasoenteric tubes without obviously visual indicators patients requiring NG or NJ feeding are required to check the position of their tube before administrating water, feed or drugs through the tube. This is done through the aspirate of a small amount of gastric or jejunal content from the tube and testing the acidity on CE marked pH indicator paper. A pH of <5.5 indicates gastric positioning and pH 6-8 indicates presence in the small bowel.
Gastrostomy feeding
A gastrostomy feeding tube is placed by a doctor through the abdominal wall into the stomach, thus bypassing the mouth and oesophagus.
This is also sometimes referred to as a PEG (percutaneous endoscopic gastrostomy) or a Button gastrostomy.
There are various ways of administering the feed:
- Bolus administers the feed solution over a 15-20 minute period several times a day;
- Intermittent gravity drip administers the feed solution over 30-60 minutes several times a day;
- Continuous administers the feed solution over a period of between 8-24 hours.
Jejunostomy feeding
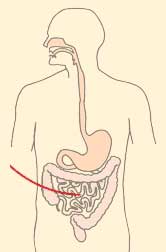 The feeding tube is inserted through the abdominal wall into the jejunum.
The feeding tube is inserted through the abdominal wall into the jejunum.
A jejunostomy feeding tube is placed by a doctor through the abdominal wall directly into a part of the small intestine called the jejunum.
This is sometimes referred to as a PEJ (Percutaneous Endoscopic Jejunostomy).
Feeding into the jejunum bypasses the mouth, oesophagus and stomach.
There are various ways of administering the feed:
- Intermittent gravity drip administers the feed solution over 30-60 minutes several times a day;
- Continuous administers the feed solution over a period of between 8-24 hours.
Total parenteral nutrition (TPN) is given via a dedicated catheter (CVC - central venous catheter) which is placed into a main vein, The tip of the catheter sits (a) close to the heart.
- insertion site of permanent catheter
- exit site of catheter with an external segment.
The implanted port is situated in the upper chest wall.
The nutrients that the body requires are in a solution which is administered intravenously through a small permanent catheter placed in a main vein. There are two types of catheter: one which has an external segment and one which is an implanted device.
The catheter must be connected to the bag of nutrient solution under aseptic conditions, as the catheter tip lies approximately 3cm from the heart. The connection procedures have been developed to ensure that the risk of allowing bacteria into the bloodstream is virtually nil.
The normal volume infused is between 2 - 3 litres, but some may need larger volumes for a longer time. It is generally given over a 10 - 12 hour period, and most people choose to do this overnight.
'Total parenteral nutrition' (TPN) is also referred to as Parenteral nutrition (PN) and 'home parenteral nutrition' (HPN). Total parenteral nutrition is the practice of feeding a person intravenously, bypassing the usual process of eating and digestion. The person receives nutritional formulas containing salts, glucose, amino acids, lipids and added vitamins. The feeding tube is connected to the bag of feed solution. The feed is then pumped in using a standard infusion pump or ambulatory pump. Ambulatory pumps give more mobility and are much lighter for patients when they are mobile i.e. on holiday, out shopping etc.. Battery-powered ambulatory infusion pumps can be used with chronic TPN patients. Usually the pump and a small (100 ml) bag of nutrient (to keep the vein open) are carried in a small bag around the waist or on the shoulder. Outpatient TPN practices are still being refined, but more and more patients are being provided with home care assistance, substantially reducing the need for acute hospital care (Which saves the NHS revenue costs and staffing, whilst also freeing up acute hospital beds.
 TPN is provided when the gastrointestinal tract is not functioning because of an interruption in its continuity or because its absorptive capacity is impaired. It has been used for comatose patients, although enteral feeding is usually preferable, and less prone to complications. Short-term TPN may be used if a person's digestive system has shut down (for instance by Peritonitis), and they are at a low enough weight to cause concerns about nutrition during an extended hospital stay. Long-term TPN is occasionally used to treat people suffering the extended consequences of an accident or surgery. Most controversially, TPN has extended the life of a small number of children born with non-existent or severely deformed guts. The preferred method of delivering TPN is with a medical infusion pump. A sterile bag of nutrient solution, between 500 mL and 4 L is provided. The pump infuses continuously over the feeding period. Feeding schedules vary, but one common regimen ramps up the nutrition over a few hours, levels off the rate for a few hours, and then ramps it down over a few more hours, in order to simulate a normal set of meal times.
TPN is provided when the gastrointestinal tract is not functioning because of an interruption in its continuity or because its absorptive capacity is impaired. It has been used for comatose patients, although enteral feeding is usually preferable, and less prone to complications. Short-term TPN may be used if a person's digestive system has shut down (for instance by Peritonitis), and they are at a low enough weight to cause concerns about nutrition during an extended hospital stay. Long-term TPN is occasionally used to treat people suffering the extended consequences of an accident or surgery. Most controversially, TPN has extended the life of a small number of children born with non-existent or severely deformed guts. The preferred method of delivering TPN is with a medical infusion pump. A sterile bag of nutrient solution, between 500 mL and 4 L is provided. The pump infuses continuously over the feeding period. Feeding schedules vary, but one common regimen ramps up the nutrition over a few hours, levels off the rate for a few hours, and then ramps it down over a few more hours, in order to simulate a normal set of meal times.
Chronic TPN is performed through a central intravenous catheter, usually in the subclavian or jugular vein. Another common practice is to use a PICC line (A peripherally inserted central catheter is a form of intravenous access that can be used for a prolonged period of time), which originates in the arm, and extends to one of the central veins, such as the subclavian. In infants, sometimes the umbilical vein is used.
Aside from their dependence on a pump, chronic TPN patients live quite normal lives.
Sources:
https://pinnt.com/Home.aspx
http://en.wikipedia.org/wiki/Parenteral_nutrition
http://www.ncbi.nlm.nih.gov/pubmed/6420340



