Modes of mechanical ventilation have evolved steadily over the many decades, increasing in complexity as technical capabilities are added to improve clinical outcomes.
 A key feature of this complexity has been the development of new targeting schemes, moving away from simple set-point targeting, where targets are pre-set by the operator; to adaptive targeting, where some targets are automatically adjusted; to optimal targeting, where the targets are automatically adjusted to maximise or minimise some desired performance characteristic; and even intelligent targeting, where automatic adjustment and selection of targets using the tools of artificial intelligence.
A key feature of this complexity has been the development of new targeting schemes, moving away from simple set-point targeting, where targets are pre-set by the operator; to adaptive targeting, where some targets are automatically adjusted; to optimal targeting, where the targets are automatically adjusted to maximise or minimise some desired performance characteristic; and even intelligent targeting, where automatic adjustment and selection of targets using the tools of artificial intelligence.
Optimum targeting schemes, have been the central feedback control mechanisms, of the most complex modes currently available. Optimisation means that there exists no better alternative to get, do, or set something, given the constraints of the mathematical model used. This kind of targeting scheme for ventilator modes is based on fairly arbitrary assumptions and pre-supposes clearly defined goals and targets, which are still topics of clinical debate.
The Modes of use for mechanical ventilation are some of the most important aspects for inspiratory support. The mode selection is based on clinician familiarity and institutional preferences, since there is a scarcity of evidence indicating that the mode affects clinical outcomes. The most frequently used forms of volume-limited mechanical ventilation are intermittent mandatory ventilation (IMV) and continuous mandatory ventilation (CMV).
A breath is one cycle of positive flow (inspiratory phase) and negative flow (expiratory phase) defined in terms of the flow-time curve. Inspiratory time is defined as the period from the start of positive flow to the start of negative flow. Expiratory time is defined as the period from the start of expiratory flow to the start of inspiratory flow. The flow-time curve is the basis for many variables related to ventilator settings.
An assisted breath is where the ventilator does some portion of the work of breathing. For constant flow inflation, work is defined as inspiratory pressure multiplied by tidal volume. Therefore, an assisted breath is identified as a breath for which airway pressure (displayed on the ventilator) rises above baseline during inspiration. An unassisted breath is one for which the ventilator simply provides the inspiratory flow demanded by the patient and pressure stays constant throughout the breath.
A ventilator assists breathing using either pressure control or volume control based on the equation of motion for the respiratory system. Providing assistance means doing work on the patient, which is accomplished by controlling either pressure or volume. A simple mathematical model describing this fact is known as the equation of motion for the passive respiratory system:
Pressure = (Elastance × Volume) + (Resistance × Flow)
In this equation, pressure, volume, and flow are all continuous functions of time. Pressure is actually a pressure difference across the system (e.g., transrespiratory pressure defined as pressure at the airway opening minus pressure on the body surface). Elastance (defined as the change in pressure divided by the associated change in volume; the reciprocal of compliance) and resistance (defined as a change in pressure divided by the associated change in flow) are parameters assumed to remain constant during a breath.
Volume control (VC) means that both volume and flow are preset prior to inspiration. In other words, the right hand side of the equation of motion remains constant while pressure changes with changes in elastance and resistance.
Pressure control (PC) means that inspiratory pressure is preset as either a constant value or it is proportional to the patient’s inspiratory effort. In other words, the left-hand side of the equation of motion remains constant while volume and flow change with changes in elastance and resistance.
Time control (TC) means that, in some rare situations, none of the main variables (pressure, volume, or flow) are preset. In this case only the inspiratory and expiratory times are preset.
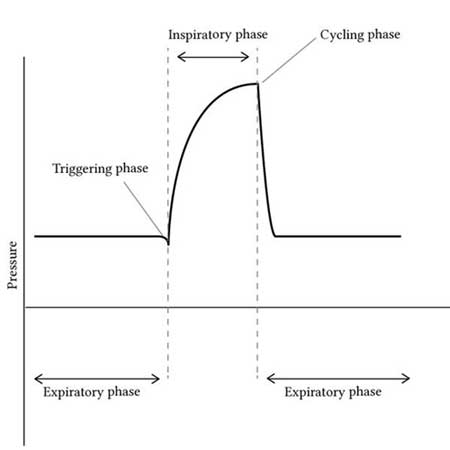
Breaths are classified by the criteria that trigger (start) and cycle (stop) inspiration. The start of inspiration is called the trigger event. The end of inspiration is called the cycle event.
Trigger and cycle events can be initiated by the patient or the machine. Inspiration can be patient triggered or patient cycled by a signal representing inspiratory effort. Inspiration may also be machine triggered or machine cycled by preset ventilator thresholds.
Patient triggering means starting inspiration based on a patient signal independent of a machine trigger signal. Machine triggering means starting inspiratory flow based on a signal from the ventilator, independent of a patient trigger signal. Patient cycling means ending inspiratory time based on signals representing the patient determined components of the equation of motion, (ie, elastance or resistance and including effects due to inspiratory effort). Flow cycling is a form of patient cycling because the rate of flow decay to the cycle threshold is determined by patient mechanics. Machine cycling means ending inspiratory time independent of signals representing the patient determined components of the equation of motion.
Breaths are classified as spontaneous or mandatory based on both the trigger and cycle events. A spontaneous breath is a breath for which the patient both triggers and cycles the breath. A spontaneous breath may occur during a mandatory breath (e.g. Airway Pressure Release Ventilation). A spontaneous breath may be assisted or unassisted. A mandatory breath is a breath for which the machine triggers and/or cycles the breath. A mandatory breath can occur during a spontaneous breath (e.g., High Frequency Jet Ventilation). A mandatory breath is, by definition, assisted.
While modes of mechanical ventilation have classically been divided up into pressure or volume controlled modes, a more modern approach describes ventilatory modes based on three characteristics – the trigger (flow versus pressure), the limit (what determines the size of the breath), and the cycle (what actually ends the breath). In both Volume Controlled Ventilation (VCV) and Pressure Controlled Ventilation (PCV), time is the cycle, the difference being in how the time to cessation is determined. Pressure Support Ventilation (PSV), by contrast, has a flow cycle.
Volume Modes
Assist-Control Ventilation (ACV) - Also known as continuous mandatory ventilation (CMV). Each breath is either an assist or control breath, but they are all of the same volume. The larger the volume, the more expiratory time required. If the I:E ratio is less than 1:2, progressive hyperinflation may result. ACV is particularly undesirable for patients who breathe rapidly – they may induce both hyperinflation and respiratory alkalosis. Note that mechanical ventilation does not eliminate the work of breathing, because the diaphragm may still be very active.
Synchronized Intermittent-Mandatory Ventilation (SIMV) - Guarantees a certain number of breaths, but unlike ACV, patient breaths are partially their own, reducing the risk of hyperinflation or alkalosis. Mandatory breaths are synchronized to coincide with spontaneous respirations. Disadvantages of SIMV are increased work of breathing and a tendency to reduce cardiac output, which may prolong ventilator dependency. The addition of pressure support on top of spontaneous breaths can reduce some of the work of breathing.
Pressure Modes
Pressure-Controlled Ventilation (PCV) - Less risk of barotrauma as compared to ACV and SIMV. Does not allow for patient-initiated breaths. The inspiratory flow pattern decreases exponentially, reducing peak pressures and improving gas exchange. The major disadvantage is that there are no guarantees for volume, especially when lung mechanics are changing. Thus, PCV has traditionally been preferred for patients with neuromuscular disease but otherwise normal lungs.
Pressure Support Ventilation (PSV) - Allows the patient to determine inflation volume and respiratory frequency (but not pressure, as this is pressure-controlled), thus can only be used to augment spontaneous breathing. Pressure support can be used to overcome the resistance of ventilator tubing in another cycle (5 – 10 cm H20 are generally used, especially during weaning), or to augment spontaneous breathing. PSV can be delivered through specialised face masks.
Pressure Controlled Inverse Ratio Ventilation (PCIRV) - Pressure controlled ventilatory mode in which the majority of time is spent at the higher (inspiratory) pressure. Early trials were promising, however the risks of auto PEEP and hemodynamic deterioration due to the decreased expiratory time and increased mean airway pressure generally outweigh the small potential for improved oxygenation.
Airway Pressure Release Ventilation (APRV) - Airway pressure release ventilation is similar to PCIRV – instead of being a variation of PCV in which the I:E ratio is reversed, APRV is a variation of CPAP that releases pressure temporarily on exhalation. This unique mode of ventilation results in higher average airway pressures. Patients are able to spontaneously ventilate at both low and high pressures, although typically most (or all) ventilation occurs at the high pressure. In the absence of attempted breaths, APRV and PCIRV are identical. As in PCIRV, hemodynamic compromise is a concern in APRV. Additionally, APRV typically requires increased sedation.
Dual Modes
Pressure Regulated Volume Control (PRVC) - A volume target backup is added to a pressure assist-control mode.
Interactive Modes
Proportional Assist Ventilation (PAV) - During PAV, the clinician sets the percentage of work of breathing to be provided by the ventilator. PAV uses a positive feedback loop to accomplish this, which requires knowledge of resistance and elastance to properly attenuate the signal.
Compliance and resistance must therefore be periodically calculated – this is accomplished by using intermittent end-inspiratory, and end-expiratory pause manoeuvres (which also calculate auto PEEP). In addition to percent support, the clinician sets the trigger and the cycle (what actually ends the breath)
The theoretical advantage of PAV is increased synchrony compared to PSV (which provides the same amount of support regardless of how much effort the patient makes)
Adaptive Support Ventilation - Calculates the expiratory time constant in order to guarantee sufficient expiratory time and thus minimize air trapping.
Positive End Expiratory Pressure (PEEP - Tube Compensation).
Positive End Expiratory Pressure (PEEP) is not a ventilatory mode in and of itself.
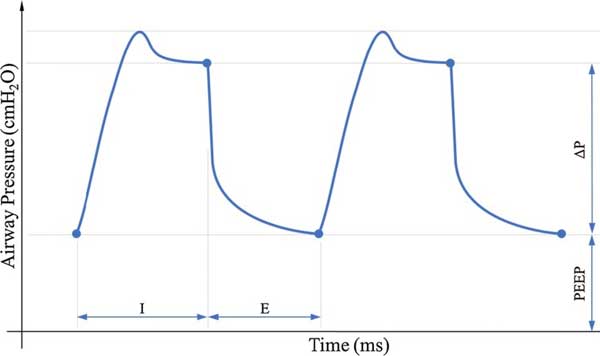
It does not allow alveolar pressure to be in equilibrium with the atmosphere. PEEP displaces the entire pressure waveform, thus mean intrathoracic pressure increases and the effects on cardiac output are amplified. Low levels of PEEP can be very dangerous, even 5 cm H20, especially in patients with hypovolemia or cardiac dysfunction. When measuring the effectiveness of PEEP, cardiac output must always be calculated because at high saturations, changes in Q will be more important than SaO2 – never use SaO2 as an endpoint for PEEP.
Continuous Positive Airway Pressure (CPAP) - Positive pressure is given throughout the cycle. It can be delivered through a mask and can be used in obstructive sleep apnoea (esp. with a nasal mask), to postpone intubation, or to treat acute exacerbations of COPD.
High Frequency Oscillatory Ventilation (HFOV) - HFOV is a lung-protective strategy that can be utilised in the full spectrum of patient populations ranging from neonatal to adults with acute lung injury. HFOV is often utilised as a rescue strategy when conventional mechanical ventilation (CV) has failed. High frequency oscillatory ventilation utilises rapid ventilation rates with small tidal volumes (often less than anatomical dead space) and active inspiratory AND expiratory phases. A constant distending airway pressure is applied to the alveoli which aims to maximise functional residual capacity and ventilation/perfusion matching, over which small tidal volumes are superimposed at a high rate. The aim of using HFOV is to reduce ventilator associated lung injury when high airway pressures and volumes in conventional ventilation modes are required to maintain adequate gas exchange. When initiated early, high frequency oscillatory ventilation may improve oxygenation and reduce risk of lung injury, especially in neonates and infants.
High Frequency Percussive Ventilation (HFPV) - HFPV combines diffusive (high frequency mini-bursts) and convective ventilation patterns. Benefits include enhanced oxygenation and hemodynamics, and alveolar recruitment, while providing hypothetic lung-protective ventilation.
https://www.openanesthesia.org/modes_of_mechanical_ventilation/
https://en.wikipedia.org/wiki/Modes_of_mechanical_ventilation
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6104409/
https://www.clinicalguidelines.scot.nhs.uk.....-a-guide-to-the-use-of-hfov-in-the-neonate/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6591785/
https://ccforum.biomedcentral.com/articles/10.1186/s13054-017-1924-6





