In hospitals there are two commonly used methods for measuring blood pressure.
- An electronic blood pressure monitor normally has an internal pump which inflates the cuff. The inflation of the cuff is monitored electronically for pulse and pressure. The machine will give an indication of blood pressure.
- A sphygmomanometer is a mechanical device used for measuring blood pressure.
Blood pressure

A sphygmomanometer.
Blood pressure (BP) is the force exerted by circulating blood on the walls of blood vessels, and constitutes one of the principal vital signs. The pressure of the circulating blood decreases as blood moves through arteries, arterioles, capillaries, and veins; the term blood pressure generally refers to arterial pressure, i.e., the pressure in the larger arteries, the blood vessels that take blood away from the heart. Arterial pressure is most commonly measured via a sphygmomanometer, which historically used the height of a column of mercury to reflect the circulating pressure. Today blood pressure values are still reported in millimetres of mercury (mmHg), though aneroid and electronic devices do not use mercury. (the UK National Health Service issued an instruction for all NHS Staff to stop using mercury devices with effect from Dec 2007)
For each heartbeat, blood pressure varies between systolic and diastolic pressures. Systolic pressure is peak pressure in the arteries, which occurs near the beginning of the cardiac cycle when the ventricles are contracting. Diastolic pressure is minimum pressure in the arteries, which occurs near the end of the cardiac cycle when the ventricles are filled with blood. An example of normal measured values for a resting, healthy adult human is 115 mmHg systolic and 75 mmHg diastolic (written as 115/75 mmHg). Pulse pressure is the difference between systolic and diastolic pressures.
Systolic and diastolic arterial blood pressures are not static but undergo natural variations from one heartbeat to another and throughout the day (in a circadian rhythm). They also change in response to stress, nutritional factors, drugs, disease, exercise, and momentarily from standing up. Sometimes the variations are large. Hypertension refers to arterial pressure being abnormally high, as opposed to hypotension, when it is abnormally low. Along with body temperature, blood pressure measurements are the most commonly measured physiological parameters.
'Normal' blood pressure varies with age, state of health and clinical situation. At birth, a typical blood pressure is 80/50 mmHg. It rises steadily throughout childhood, so that in a young adult it might be 120/80 mmHg. As we get older, blood pressure continues to rise and a rule of thumb is that normal systolic pressure is age in years +100. Blood pressure is lower in late pregnancy and during sleep.
From this, you can see that a systolic pressure of 160mmHg for an elderly man or 90 mmHg for a pregnant woman may be quite normal. To judge whether any particular reading is too high or too low, we must compare the reading with the 'normal' for that patient.
Types of blood pressure measurement
Arterial pressures can be measured invasively (by penetrating the skin and measuring inside the blood vessels) or non-invasively. The former is usually restricted to a hospital setting.
Noninvasive measurement
The noninvasive auscultatory (from the Latin for listening) and oscillometric measurements are simpler and quicker than invasive measurements, require less expertise in fitting, have virtually no complications, and are less unpleasant and painful for the patient. However, non-invasive measures may yield somewhat lower accuracy and small systematic differences in numerical results. Non-invasive measurement methods are more commonly used for routine examinations and monitoring.
Palpation methods
A minimum systolic value can be roughly estimated without any equipment by palpation, most often used in emergency situations. Palpation of a radial pulse indicates a minimum blood pressure of 80 mmHg, a femoral pulse indicates at least 70 mmHg, and a carotid pulse indicates a minimum of 60 mmHg. However, one study indicated that this method was not accurate enough and often overestimated patients' systolic blood pressure. A more accurate value of systolic blood pressure can be obtained with a sphygmomanometer and palpating for when a radial pulse returns. The diastolic blood pressure can not be estimated by this method.
Auscultatory methods
 The auscultatory method uses a stethoscope and a sphygmomanometer. This comprises an inflatable cuff placed around the upper arm at roughly the same vertical height as the heart, attached to a mercury or aneroid manometer. The mercury manometer, considered to be the gold standard for arterial pressure measurement, measures the height of a column of mercury, giving an absolute result without need for calibration, and consequently not subject to the errors and drift of calibration which affect other methods.
The auscultatory method uses a stethoscope and a sphygmomanometer. This comprises an inflatable cuff placed around the upper arm at roughly the same vertical height as the heart, attached to a mercury or aneroid manometer. The mercury manometer, considered to be the gold standard for arterial pressure measurement, measures the height of a column of mercury, giving an absolute result without need for calibration, and consequently not subject to the errors and drift of calibration which affect other methods.
The use of mercury manometers is often required in clinical trials and for the clinical measurement of hypertension in high risk patients, such as pregnant women.
A cuff of appropriate size is fitted and inflated manually by repeatedly squeezing a rubber bulb until the artery is completely occluded. Listening with the stethoscope to the brachial artery at the elbow, the examiner slowly releases the pressure in the cuff. When blood just starts to flow in the artery, the turbulent flow creates a "whooshing" or pounding (first Korotkoff sound). The pressure at which this sound is first heard is the systolic blood pressure. The cuff pressure is further released until no sound can be heard (fifth Korotkoff sound), at the diastolic arterial pressure. Sometimes, the pressure is palpated (felt by hand) to get an estimate before auscultation.
Oscillometric methods
 Oscillometric methods are sometimes used in the long-term measurement and sometimes in general practice. The equipment is functionally similar to that of the auscultatory method, but with an electronic pressure sensor (transducer) fitted in to detect blood flow, instead of using the stethoscope and the expert's ear. In practice, the pressure sensor is a calibrated electronic device with a numerical readout of blood pressure. To maintain accuracy, calibration must be checked periodically, unlike the inherently accurate mercury manometer. In most cases the cuff is inflated and released by an electrically operated pump and valve, which may be fitted on the wrist (elevated to heart height), although the upper arm is preferred. They vary widely in accuracy, and should be checked at specified intervals and if necessary recalibrated.
Oscillometric methods are sometimes used in the long-term measurement and sometimes in general practice. The equipment is functionally similar to that of the auscultatory method, but with an electronic pressure sensor (transducer) fitted in to detect blood flow, instead of using the stethoscope and the expert's ear. In practice, the pressure sensor is a calibrated electronic device with a numerical readout of blood pressure. To maintain accuracy, calibration must be checked periodically, unlike the inherently accurate mercury manometer. In most cases the cuff is inflated and released by an electrically operated pump and valve, which may be fitted on the wrist (elevated to heart height), although the upper arm is preferred. They vary widely in accuracy, and should be checked at specified intervals and if necessary recalibrated.
Oscillometric measurement requires less skill than the auscultatory technique, and may be suitable for use by untrained staff and for automated patient home monitoring.
The cuff is inflated to a pressure initially in excess of the systolic arterial pressure, and then reduces to below diastolic pressure over a period of about 30 seconds. When blood flow is nil (cuff pressure exceeding systolic pressure) or unimpeded (cuff pressure below diastolic pressure), cuff pressure will be essentially constant. It is essential that the cuff size is correct: undersized cuffs may yield too high a pressure, whereas oversized cuffs yield too low a pressure. When blood flow is present, but restricted, the cuff pressure, which is monitored by the pressure sensor, will vary periodically in synchrony with the cyclic expansion and contraction of the brachial artery, i.e., it will oscillate. The values of systolic and diastolic pressure are computed, not actually measured from the raw data, using an algorithm; the computed results are displayed.
Oscillometric monitors may produce inaccurate readings in patients with heart and circulation problems, that include arterial sclerosis, arrhythmia, preeclampsia, pulsus alternans, and pulsus paradoxus.
In practice the different methods do not give identical results; an algorithm and experimentally obtained coefficients are used to adjust the oscillometric results to give readings which match the auscultatory results as well as possible. Some equipment uses computer-aided analysis of the instantaneous arterial pressure waveform to determine the systolic, mean, and diastolic points. Since many oscillometric devices have not been validated, caution must be given as many are not suitable for use in clinical and acute care settings.
The term NIBP, for Non-Invasive Blood Pressure, is often used to describe oscillometric monitoring equipment.
When measuring blood pressure, an accurate reading requires that one not drink coffee, smoke cigarettes, or engage in strenuous exercise for 30 minutes before taking the reading. A full bladder may have a small effect on blood pressure readings. The blood pressure cuff should always be against bare skin, as readings taken over a shirt sleeve are less accurate. During the reading, the arm that is used should be relaxed and kept at heart level, for example by resting it on a table. Since arterial pressure varies throughout the day, measurements intended to monitor changes over longer time frames should be taken at the same time of day to ensure that the readings are comparable.
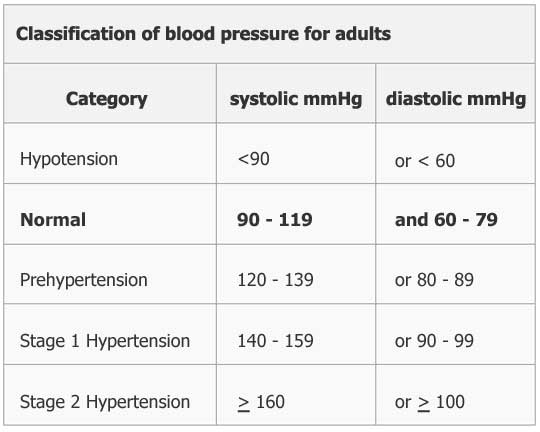
The following classification of blood pressure applies to adults aged 18 and older. It is based on the average of seated blood pressure readings that were properly measured during 2 or more office visits.
Normal values
While average values for arterial pressure could be computed for any given population, there is often a large variation from person to person; arterial pressure also varies in individuals from moment to moment. Additionally, the average of any given population may have a questionable correlation with its general health, thus the relevance of such average values is equally questionable. However, in a study of 100 subjects with no known history of hypertension, an average blood pressure of 112/64 mmHg was found, which is in the normal range. In children the normal ranges are lower than for adults. In the elderly, blood pressure tends to be higher than normal adult values, largely because of reduced flexibility of the arteries.
The risk of cardiovascular disease increases progressively throughout the range of higher arterial pressure that begins at 115/75 mmHg. In the past, hypertension was only diagnosed if secondary signs of high arterial pressure were present, along with a prolonged high systolic pressure reading over several visits. In the US, this reactive stance has been soundly rejected in light of recent evidence. However in the UK, patients' readings are still considered normal up to 140/90 mmHg.
Clinical trials demonstrate that people who maintain arterial pressures at the low end of these pressure ranges have much better long term cardiovascular health. The principal medical debate concerns the aggressiveness and relative value of methods used to lower pressures into this range for those who do not maintain such pressure on their own. Elevations, more commonly seen in older people, though often considered normal, are associated with increased morbidity and mortality. The clear trend from double blind clinical trials (for the better strategies and agents) demonstrates that lower arterial pressure correlates with lower rates of disease.
Compiled and edited by: John Sandham IEng MIET
Sources:
https://www.ndcn.ox.ac.uk/
http://www.bloodpressureuk.org/Home
http://en.wikipedia.org/wiki/Blood_pressure




