Non-invasive ventilation refers to the delivery of mechanical ventilation to the lungs using techniques that do not require an endotracheal airway. A non-invasive ventilator is used to support breathing with the ventilation being administered through a face mask, nasal mask, or a helmet.
It is called "non-invasive" because it is delivered with a mask that is tightly fitted to the face or around the head, but without a need for tracheal intubation (a tube that goes in the mouth and continues down into the patient’s windpipe). While there are similarities with regards to the interface, non-invasive ventilation is not the same as continuous positive airway pressure (CPAP), which applies a single level of positive airway pressure throughout the whole respiratory cycle; CPAP does not deliver ventilation but is occasionally used in conditions also treated with non-invasive ventilation.
Air, usually with added oxygen, is given through the mask under positive pressure generated from either an internal electrical air pump, or by use of piped gases (air and oxygen) and internal mechanical controls. The amount of pressure in the mask is alternated, dependent upon the normal breathing rate and lung volume for that particular patient. Each ventilator is individually set at the most appropriate clinical settings for the patient being ventilated.
Non-invasive ventilation is used in acute respiratory failure caused by a number of medical conditions, most prominently chronic obstructive pulmonary disease (COPD); numerous studies have shown that appropriate use of non-invasive ventilation reduces the need for invasive ventilation and its complications. Furthermore, it may be used on a long-term basis in people who cannot breathe independently as a result of a chronic condition.
History of non-invasive ventilation
 The concept of mechanical ventilation first evolved with negative-pressure ventilation. In 1876, Woillez first developed a workable iron lung. In 1889, Alexander Graham Bell designed and built a prototype of iron lung for use with a newborn infant. In the late 1920s, Drinker introduced negative-pressure ventilation and popularized the iron lung.
The concept of mechanical ventilation first evolved with negative-pressure ventilation. In 1876, Woillez first developed a workable iron lung. In 1889, Alexander Graham Bell designed and built a prototype of iron lung for use with a newborn infant. In the late 1920s, Drinker introduced negative-pressure ventilation and popularized the iron lung.
He maintained an 8-year-old girl with acute poliomyelitis on artificial respiration continuously for 122 hours. The polio epidemics of the 1930s, 1940s, and 1950s led to the development of pulmonary medicine as a specialty and the iron lung as a workhorse. Ventilators delivering negative-pressure ventilation fell out of favour as the use of invasive positive-pressure ventilation (PPV) increased during the 1960s. However, over the past decade, a striking resurgence has been observed in the use of non-invasive ventilation, fuelled by the development of PPV delivered through a nasal or face mask.
By the 1960s invasive (i.e. via an endotracheal tube) positive pressure ventilation superseded negative pressure ventilation, primarily because of better airway protection. The past decade has seen a resurgence in the use of non-invasive ventilation, largely because of the development of nasal ventilation, which has the potential of providing ventilatory assistance with greater convenience, comfort, safety, and less cost than invasive ventilation.
Fixed-pressure CPAP
(Continuous Positive Airway Pressure)
 A continuous positive airway pressure (CPAP) machine was initially used mainly by patients for the treatment of sleep apnoea at home, but now is in widespread use across intensive care units as a form of ventilation. Obstructive sleep apnoea occurs when the upper airway becomes narrow as the muscles relax naturally during sleep. This reduces oxygen in the blood and causes arousal from sleep. The CPAP machine stops this phenomenon by delivering a stream of compressed air via a hose to a nasal pillow, nose mask or full-face mask, splinting the airway (keeping it open under air pressure) so that unobstructed breathing becomes possible, reducing and/or preventing apnoea’s and hypopneas.
A continuous positive airway pressure (CPAP) machine was initially used mainly by patients for the treatment of sleep apnoea at home, but now is in widespread use across intensive care units as a form of ventilation. Obstructive sleep apnoea occurs when the upper airway becomes narrow as the muscles relax naturally during sleep. This reduces oxygen in the blood and causes arousal from sleep. The CPAP machine stops this phenomenon by delivering a stream of compressed air via a hose to a nasal pillow, nose mask or full-face mask, splinting the airway (keeping it open under air pressure) so that unobstructed breathing becomes possible, reducing and/or preventing apnoea’s and hypopneas.
It is important to understand, however, that it is the air pressure, and not the movement of the air, that prevents the apnoea’s. When the machine is turned on, but prior to the mask being placed on the head, a flow of air comes through the mask. After the mask is placed on the head, it is sealed to the face and the air stops flowing. At this point, it is only the air pressure that accomplishes the desired result. This has the additional benefit of reducing or eliminating the extremely loud snoring that sometimes accompanies sleep apnoea.
 The CPAP machine blows air at a prescribed pressure (also called the titrated pressure). The necessary pressure is usually determined by a sleep physician after review of a study supervised by a sleep technician during an overnight study (polysomnography) in a sleep laboratory. The titrated pressure is the pressure of air at which most (if not all) apnoea’s and hypopneas have been prevented, and it is usually measured in centimetres of water (cm H2O).
The CPAP machine blows air at a prescribed pressure (also called the titrated pressure). The necessary pressure is usually determined by a sleep physician after review of a study supervised by a sleep technician during an overnight study (polysomnography) in a sleep laboratory. The titrated pressure is the pressure of air at which most (if not all) apnoea’s and hypopneas have been prevented, and it is usually measured in centimetres of water (cm H2O).
The pressure required by most patients with sleep apnoea ranges between 6 and 14 cm H2O. A typical CPAP machine can deliver pressures between 4 and 20 cm H2O. More specialized units can deliver pressures up to 25 or 30 cm H2O. CPAP treatment can be highly effective in treatment of obstructive sleep apnoea. For some patients, the improvement in the quality of sleep and quality of life due to CPAP treatment will be noticed after a single night's use.
Often, the patient's sleep partner also benefits from markedly improved sleep quality, due to the amelioration of the patient's loud snoring. Given that sleep apnoea is a chronic health issue and doesn't go away, ongoing care is needed to maintain CPAP therapy. Based on the study of cognitive behavioural therapy (referenced above), ongoing chronic care management is the best way to help patients continue therapy by educating them on the health risks of sleep apnoea and providing motivation and support.
APAP or AutoPAP or AutoCPAP
APAP or AutoPAP or AutoCPAP (Automatic Positive Airway Pressure) automatically titrates, or tunes, the amount of pressure delivered to the patient to the minimum required to maintain an unobstructed airway on a breath-by-breath basis by measuring the resistance in the patient's breathing, thereby giving the patient the precise pressure required at a given moment and avoiding the compromise of fixed pressure.
Bi-level pressure devices
VPAP or BiPAP (Variable/Bilevel Positive Airway Pressure) provides two levels of pressure: Inspiratory Positive Airway Pressure (IPAP) and a lower Expiratory Positive Airway Pressure (EPAP) for easier exhalation. (Some people use the term BPAP to parallel the terms APAP and CPAP.)
Modes S (Spontaneous) - In spontaneous mode the device triggers IPAP when flow sensors detect spontaneous inspiratory effort and then cycles back to EPAP.
T (Timed) - In timed mode the IPAP/EPAP cycling is purely machine-triggered, at a set rate, typically expressed in breaths per minute (BPM).
S/T (Spontaneous/Timed) - Like spontaneous mode, the device triggers to IPAP on patient inspiratory effort. But in spontaneous/timed mode a "backup" rate is also set to ensure that patients still receives a minimum number of breaths per minute if they fail to breathe spontaneously.
Modes of non-invasive ventilation
Negative-pressure ventilation
Negative-pressure ventilators support ventilation by lowering the pressure surrounding the chest wall during inspiration and reversing the pressure to atmospheric level during expiration. These devices augment the tidal volume by generating negative extrathoracic pressure. Several of these devices, such as body ventilators and iron lungs, are available and either cover the whole body below the neck or apply negative pressure to the thorax and abdomen.
The role of negative-pressure ventilation in the management of acute respiratory failure is unclear. Although studies of body ventilators have shown benefit in patients with chronic obstructive pulmonary disease (COPD), neuromuscular disease, and chest wall deformities who develop acute respiratory failure, prospective and controlled studies are lacking. These devices are not readily accepted by patients because of their awkward size and their propensity to cause upper airway obstructions in some patients. Several uncontrolled studies reported benefits of intermittent negative-pressure ventilation in patients with chronic respiratory failure resulting from chest wall, neuromuscular, or central hypoventilation. However, no benefit was demonstrated in patients with stable but severe COPD.
CPAP
 CPAP by nasal mask provides a pneumatic splint which holds the upper airway open in patients with nocturnal hypoxaemia due to episodes of obstructive sleep apnoea. It provides positive airway pressure throughout all phases of spontaneous ventilation. CPAP increases the FRC and opens collapsed alveoli. CPAP reduces left ventricular transmural pressure and therefore increases cardiac output. Hence it is a very effective for treatment of pulmonary oedema. Pressures are usually limited to 5-12 cm of H2O, since higher pressure tends to result in gastric distension requiring continual aspiration through a nasogastric tube.
CPAP by nasal mask provides a pneumatic splint which holds the upper airway open in patients with nocturnal hypoxaemia due to episodes of obstructive sleep apnoea. It provides positive airway pressure throughout all phases of spontaneous ventilation. CPAP increases the FRC and opens collapsed alveoli. CPAP reduces left ventricular transmural pressure and therefore increases cardiac output. Hence it is a very effective for treatment of pulmonary oedema. Pressures are usually limited to 5-12 cm of H2O, since higher pressure tends to result in gastric distension requiring continual aspiration through a nasogastric tube.
BIPAP
Bilevel positive airway pressure provides two levels of positive pressure. During exhalation, pressure is variably positive. Airflow in the circuit is sensed by a transducer and augmented to a preset level of ventilation. Cycling between inspiratory and expiratory modes may either be triggered by the patient's breaths or preset.
Volume limited ventilation
In this mode, ventilators are usually set in assist-control mode with high tidal volume (10-15 ml/kg) to compensate for air leaks. This mode is suitable for patients with obesity or chest wall deformity (need high inflation pressure) and in patients with neuromuscular diseases who need high tidal volumes for ventilation.
Proportional assist ventilation (PAV)
This is a newer mode of ventilation. In this mode the ventilator has the capacity for responding rapidly to the patients' ventilatory efforts. By adjusting the gain on the flow and volume signals, one can select the proportion of breathing work that is to be assisted.
The BIPAP ventilator has been used in randomized trials with good results. However, the conventional ventilator offers a number of advantages, such as the delivery of precise oxygen concentrations and separate inspiratory and expiratory tubing that minimizes carbon dioxide rebreathing. Patient disconnection can be readily detected because monitoring and alarm features are more sophisticated in conventional ventilators than in bi-level systems.
Advantages and Disadvantages of Non-Invasive Ventilation
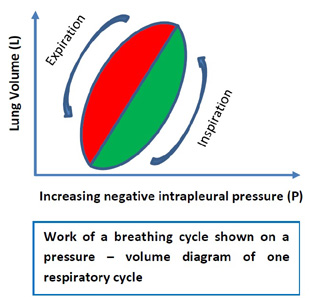
The work of breathing equals the product of pressure change across the lung and volume of gas moved. During inspiration, most of the work is done to overcome elastic recoil of the thorax and lungs, and the resistance of the airways and non-elastic tissues. For years, negative pressure ventilators were the only non-invasive methods of assisting ventilation. It was later recognized that delivery of continuous positive airway pressure by close fitting nasal masks for treatment of obstructive sleep apnoea could also be used to deliver an intermittent positive pressure. This was followed by improvements in the interface and establishment of role of NIV in patients with COPD. The use of NIV has increased in the last decade in various conditions to avoid the complications of intubation.
Advantages
- Preservation of airway defence mechanism
- Early ventilatory support
- Intermittent ventilation
- Patient can eat, drink and communicate
- Ease of application and removal
- Patient can cooperate with physiotherapy
- Improved patient comfort
- Reduced sedation requirements
- Avoidance of complications of intubation
- Ventilation outside hospital setting possible
Disadvantages
- Mask is uncomfortable/claustrophobic
- Time consuming for medical and nursing staff
- Airway is not protected
- No direct access to bronchial tree for suction
Mechanism of Action
- Improvement in pulmonary mechanics and oxygenation NIV augments alveolar ventilation and allows oxygenation without raising the PaCO2.
- Partial unloading of respiratory muscles NIV reduces trans-diaphragmatic pressure, pressure time index of respiratory muscles and diaphragmatic electromyographic activity. This leads to an increase in tidal volume, decrease in respiratory rate and increase in minute ventilation. Also overcomes the effect of intrinsic PEEP.
- Resetting of respiratory centre ventilatory responses to PaCO2 In patients with COPD, the ventilatory response to raised PaCO2 is decreased especially during sleep. By maintaining lower nocturnal PaCO2 during sleep by administering NIV, it is possible to reset the respiratory control centre to become more responsive to an increased PaCO2 by increasing the neural output to the diaphragm and other respiratory muscles. These patients are then able to maintain a more normal PaCO2 throughout the daylight hours without the need for mechanical ventilation. The carotid bodies are small structures, situated above the carotid bifurcation on each side. They are involved in the chemical control of breathing, by acting as chemoreceptors, being sensitive to levels of oxygen and carbon dioxide in the blood. There is evidence that suggests that carotid bodies are also sensitive to changes in blood pressure, blood flow and blood osmolarity.
The use of NIV has increased during the past few years. In acute exacerbation of COPD it is now considered the ventilator mode of first choice. For treatment of acute pulmonary oedema, CPAP alone is very effective. NIV reduces the chances of endotracheal intubation in hypoxemic respiratory failure. It is also being used to facilitate weaning from invasive ventilation. NIV is first choice in patients with neuromuscular diseases and chest wall deformity. Central hypoventilation and patients of obstructive sleep apnoea not responding to CPAP are also acceptable indications.
Risks associated with non-invasive ventilation
Non-invasive ventilation (NIV) is increasingly being used in acute hospitals and a recent NHS audit has highlighted the importance of giving NIV in an appropriate environment by appropriately trained staff. A particular risk relating to the delivery of NIV has been identified. A serious incident reported to the National Reporting and Learning System (NRLS)
described that a mask for non-invasive ventilation (NIV) was attached to a patient’s face but the ventilation machine had not been switched on. The patient became severely hypoxic and died. A similar case has also been reported to MHRA.
A review of NRLS data since 2012 identified three additional fatal incidents in which the oxygen supply was found to be disconnected when patients were receiving NIV. In these cases, the length of time that the oxygen tubing was detached was unknown as no regular checking of oxygen tubing was completed, and no patient observations were recorded.
Unlike ventilators that provide life-sustaining ventilation, non-invasive ventilators may lack features to warn staff of delivery problems, such as disconnection and loss of gas supply. Where devices delivering NIV have an alarm facility, this function has sometimes been disabled by staff. Devices also differ in their modes of operation; for example, following a pause in NIV therapy, some machines automatically revert to ventilation support when the mask is re-fitted; others need to be manually reactivated.
Review of incidents reported to the NRLS suggest that risks are increased when:
- patients, especially those with limited ability to summon help, are not closely monitored
- staff are not familiar with the equipment and its correct use (e.g. unclear about when to use vented or non-vented masks, or patients bringing devices from home)
- a new make and model of device is implemented; staff, even when they have been trained on the new device, may instinctively expect the device to work in the same way as the previous make and model in use.
Sources:
https://www.england.nhs.uk/wp-content/uploads/2015/02/psa-niv.pdf
https://www.nhs.uk/conditions/chronic-obstructive-pulmonary-disease-copd/treatment/
http://www.frca.co.uk/article.aspx?articleid=100430
http://emedicine.medscape.com/article/304235-overview
http://ajrccm.atsjournals.org/cgi/content/full/163/2/540
https://en.wikipedia.org/wiki/Non-invasive_ventilation
Edited by John Sandham