Nellcor UK Training Programme
Nellcor is a division of Tyco Healthcare
- Introduction
- Objectives
- Review of Oxygen Transport Physiology
- How Oxygen enters the blood
- How Oxygen is carried in the blood
- Total Oxygen content
- Arterial Oxygen Saturation
- Anaemia
- Oxyhaemoglobin Dissociation Curve
- 2,3 DPG
- Shifting of the ODC
- Hypoxaemia
- Hypoxaemia: New Terminology
- Patients at risk for Hypoxaemia
- Hypoxaemia: Clinical & Economic significance
- Hypoxaemia: Traditional Assesment
- Technology
- Accuracy
- Inovations in technology
- SAT seconds alarm management
- Optimizing Pulse Oximetry
- Detection of Hypoxaemia
- Sensor selection & use
- Maintenance and care
- Test
- References
Nellcor UK Training Programme
Nellcor is a division of Tyco Healthcare
Introduction
Pulse oximetry has provided a safe and simple method of assessing a patient's arterial blood oxygenation since the early 1980s. Around this time, pulse oximetry monitoring was initiated in the anaesthesia setting in an effort to optimize patient safety. The goal was to minimize unrecognized episodes of hypoxaemia associated with growing malpractice claims. Episodes of hypoxaemia diminished during this adoption period; and the use of pulse oximetry expanded to various inpatient care settings, such as post-anaesthesia care, critical care and the general care floor. Today, pulse oximetry reaches many healthcare arenas, including subacute care, long-term care, outpatient clinics, procedure areas, physician offices and the home.
Understanding the information that a pulse oximeter provides, and making appropriate assessments and decisions about patient oxygenation, improves patient care. This improved care is evident in two areas: First, by allowing early identification of hypoxaemic episodes that can impact patient safety; second, by facilitating clinical management of the patient. This training programme is intended to support the understanding of critical clinical concepts related to pulse oximetry, and support appropriate applications of this technology.
Objectives
By the end of this training programme, you will be able to:
- Describe how oxygen is carried in the blood.
- Define the relationship of oxygen saturation to total oxygen content.
- Review the clinical significance and incidence of hypoxemia.
- Discuss the basics of pulse oximetry technology.
- Review three factors that may cause arterial blood oxygen saturation (SpO2) to differ from arterial hemoglobin oxygen saturation (Sa02).
- Analyze the utility of the SpO2 value in patients with anemia, dysfunctional hemoglobin, venous pulsations and edema.
- Describe three considerations for sensor selection for patients being monitored with pulse oximetry.
- Identify the role of pulse oximetry in monitoring patients for hypoxemia.
- Identify three possible applications for the use of pulse oximetry in your clinical setting.
Review of Oxygen Transport Physiology
To ensure adequate oxygenation, several physiologic mechanisms must occur:
- The blood must have adequate amounts of oxygen.
- There must be adequate amounts of oxygen carriers, or hemoglobin molecules.
- There must be adequate cardiac output to carry the oxygen to the tissues.
- The cells must be able to adequately use the oxygen that is delivered.
This training programme focuses on the first two mechanisms of ensuring adequate oxygenation.
How Oxygen enters the blood
During inspiration, oxygen from the air around us enters the airways and is transported down to the alveoli (air sacs) in our lungs. Because the concentration, or partial pressure of oxygen in the alveoli, is higher than in the pulmonary capillaries, the oxygen moves across the alveoli. It then enters the pulmonary capillary bloodstream for transport to the tissues in our body. This movement of oxygen from an area of higher concentration to an area of lower concentration is called "diffusion."
How Oxygen is carried in the blood
Once oxygen enters the blood, it is carried in two forms. A small amount of oxygen is dissolved in the arterial plasma, and is measured and reported as PaO2, which represents the partial pressure of oxygen in the arterial plasma. About 1% to 2% of all oxygen present in the blood is carried this way. However, because the oxygen concentration dissolved in the blood is so high, much of the oxygen moves from the plasma and is carried bound to hemoglobin molecules. Haemoglobins are proteins in the red blood cells.

This combined oxygen and haemoglobin is referred to as "oxyhaemoglobin." Haemoglobin not bound with anything is called "deoxyhaemoglobin" or "reduced haemoglobin." Normally, 98% to 99% of oxygen in the blood is carried as oxyhaemoglobin. Oxygen carried on the arterial haemoglobin is measured and reported as Sa02, which is the arterial haemoglobin oxygen saturation.
Total Oxygen Content

The amount of oxygen dissolved in plasma is an important determinant of the amount of oxygen that is bound with haemoglobin. When there are adequate amounts of oxygen dissolved in the plasma, normally there are greater amounts of oxygen bound with haemoglobin molecules. When inadequate amounts of oxygen are dissolved in the plasma, there may be less oxygen combining with haemoglobin molecules. Therefore, both PaO2 and Sa02 are important indicators of blood oxygenation. However, most of the total arterial blood oxygen content is attributed to the oxygen combined with haemoglobin.
ARTERIAL OXYGEN SATURATION
Arterial haemoglobin oxygen saturation is often determined by a measurement of an arterial blood sample, and reported as Sa02. The saturation of haemoglobin is the ratio of the number of oxyhaemoglobin molecules to the total number of haemoglobin molecules available to bind with oxygen. This number is expressed as a percentage.


A pulse oximeter also measures arterial blood saturation. This measurement is often reported as SpO2.
The normal patient range for any arterial haemoglobin saturation,whether Sa02 or SpO2 is 95% to 99%
Anaemia
Haemoglobin values must be considered when assessing the adequacy of arterial oxygen content. The anaemic patient may have the same normal Sa02 or SpO2 levels as a patient with a normal haemoglobin value.
Although all of the haemoglobin molecules are carrying oxygen, the anaemic patient has fewer haemoglobin molecules. The total arterial oxygen content in this patient's blood is therefore lower. The anaemic patient may be at greater risk whenever oxygen demand increases or oxygen supply decreases.
| Hb content ~ 15 gm/dl SpO2 = 100% |  |
| Hb content ~ 8 gm/dl SpO2 = 100% |  |
| Hb content < 15 gm/dl SpO2 = ? % |  |
The Oxyhaemoglobin Dissociation Curve
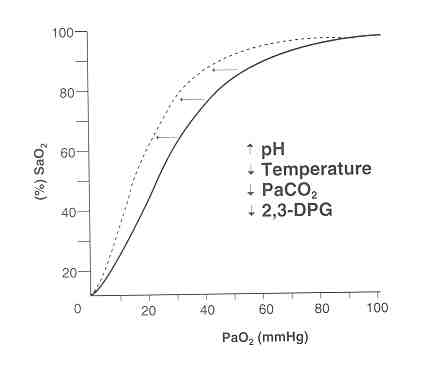
The oxyhaemoglobin dissociation curve (ODC) is a graphic relationship between haemoglobin oxygen saturation and the partial pressure of oxygen in the blood.
The affinity of haemoglobin for oxygen produces an S-shaped curve representing the way oxygen normally loads onto, and releases from, the haemoglobin molecules. The flat upper portion represents oxygen loading of haemoglobin as blood passes through the lungs. Because the partial pressure of oxygen is high, oxygen binds with the haemoglobin molecule. However, because most haemoglobin molecules are already saturated, additional loading of oxygen onto haemoglobin will not significantly increase as partial pressure continues to increase. The steep lower portion of the curve represents the relationship at the tissue level. Haemoglobin molecules are not well saturated because they have already lost some of their oxygen to tissues. Even with minor reductions in the partial pressure of oxygen, large amounts of oxygen are off-loaded from haemoglobin molecules.
The Normal ODC
The normal ODC, as shown, represents the relationship between changes in haemoglobin saturation and partial pressure of oxygen under certain "normal" conditions.

These include a blood pH of 7.4, PaCO2 of 40mmHG, temperature of 37oC, and normal levels of 2,3-DPG.
2,3-DPG
2,3-DPG is a normal product of red blood cell metabolism. Because of its chemical characteristics, 2,3-DPG plays an important physiologic role in regulating affinity between haemoglobin and oxygen. Some conditions will increase the metabolic production of 2,3-DPG, resulting in decreased affinity of haemoglobin for oxygen. Other conditions, listed in the chart below, may result in lower levels of 2,3-DPG and an increased affinity of haemoglobin for oxygen.
| Increased 2,3-DPG | Decreased 2,3-DPG |
| Residence at high altitudes | Stored blood bank |
| Anaemia | Hypophosphatemia |
| Chronic hypoxemia | Hypothyroidism |
| Hyperthyroidism |
SHIFTING OF THE ODC
Under conditions where pH, temperature, PaCO2 and 2,3-DPG are normal, a partial pressure of oxygen at 60 mmHg corresponds with an oxygen saturation value of approximately 90%. However since many patients have altered pH, PaCO2, temperature and/or 2,3-DPG values, this normal relationship may be altered. In this scenario, ODC is described as being "shifted." These curve shifts reflect altered affinity of haemoglobin for oxygen, which affects oxygen loading and unloading. Normal PaO2/Sa02 correlation is affected when the curve is shifted.
Right Shift
A right shift in the ODC decreases haemoglobin's affinity for oxygen.
Haemoglobin does not hold onto oxygen as tightly, and off-loading of oxygen is easier.
| Factors causing a Right ODC Shift |
Clinical Conditions Causing a Right ODC Shift |
| Decreased pH | Acidosis |
| Increased temperature | Hyperthermia |
| Increased PaCO2 | Alveolar hyperventilation |
| Increased 2,3-DPG | Anemia |

Left Shift
A left shift in the ODC increases haemoglobin's affinity for oxygen.
Haemoglobin has a tighter hold on oxygen and off-loading of oxygen is more difficult.
| Factors causing a Left ODC Shift |
Clinical Conditions Causing a Left ODC Shift |
| Increased pH | Alkalosis |
| Decreased temperature | Hypothermia |
| Decreased PaCO2 | Hyperventilation |
| Decreased 2,3-DPG | Carboxyhemoglobinemia, hypophosphatemia, fetal hemoglobin |
Hypoxaemia: The Incidence and Clinical Significance
Recently, a growing body of research has examined the incidence and significance of hypoxaemia. Although this research base continues to grow, there have been many relevant findings related to risk factors for hypoxaemia and its potential consequences.
HYPOXAEMIA: NEW TERMINOLOGY
"Hypoxaemia" refers to insufficient oxygenation of the arterial blood. Hypoxaemia may lead to "hypoxia," or insufficient oxygenation of the tissues. The consequences of hypoxia can include serious tissue damage, brain damage, and even death. A priority of any healthcare provider is to prevent hypoxaemia and ensure adequate oxygenation of patients.
Hypoxaemia can occur in an episodic or constant fashion. Episodic hypoxaemia is occasionally present and is characterized by sudden changes in Sa02. The degree of episodic hypoxaemia may be mild, moderate or severe. For example, patients may have an episodic hypoxaemic event while traveling from the bed to the bathroom, or while climbing stairs in their home. During these episodic events, patients may not have enough oxygen available to meet the metabolic demands required by this activity.
Patients with constant hypoxaemia are those who have consistently low oxygen saturation readings. The degree of constant hypoxaemia can vary. Constant hypoxaemia is often associated with chronic medical conditions, such as chronic obstructive lung disease or cyanotic heart disease.
PATIENTS AT RISK FOR HYPOXAEMIA
Certain patient populations are at greater risk for hypoxaemia and should be considered candidates for continuous monitoring of hypoxaemia with pulse oximetry. These patient populations include:
| Patients at risk for Hypoxaemia | Risk Factors |
| Patients in Noncritical Care Settings (Hospitals and Alternate Care). | Patients cared for in non-critical care areas have complex medical and surgical conditions, which may directly or indirectly affect their cardio-respiratory status. Patient assessment by staff may be less frequent, and patients may be physically located away from the watchful eyes of the caregiver. A decrease in the use of monitoring technologies in these settings may result in hypoxaemia being underestimated. |
| Postoperative Patients | Episodic postoperative hypoxaemia can occur in the first few hours after surgery. It can also occur up to five nights postoperatively. It can also be associated with sudden unexplained death. Postoperative patients may be at risk for poor oxygenation because of residual effects of anaesthesia, pain-inhibited respiratory movement, analgesic induced respiratory depression and bed rest. Patients who have had major abdominal or thoracic surgeries, or any surgery in the upper airway area, are considered high risk. In addition, those with a significant perioperative oxygenation defect or pre-existing pulmonary disease may be at greater risk during the postoperative period. |
| Patients in Pain/Receiving Pain Management | Both pain and pain management can contribute to hypoxaemia. Pain can inhibit expansion of the chest wall, and interfere with patient activity and mobility. Pain management has the potential to cause respiratory depression. The Agency for Healthcare Policy and Research clinic guidelines related to pain management recommend opioids as the drug of choice, with frequent mention of respiratory depression as a serious complication of opioid use. |
| Confirmed Obstructive Sleep Apnoea or Morbidly Obese Patients |
Patients often receive little or no assessment of their sleep habits for apnoea, yet the presence of sleep apnoea is clearly associated with the development of hypoxaemia. In the postoperative period, a rebound in REM sleep days after surgery may be a contributing factor to the development of late postoperative hypoxaemia. Since hypoventilation is a major respiratory side effect of opiate administration, patients with sleep apnoea who receive opioids for pain management may be at greater risk for apnea-associated hypoxaemia. However, patients who undergo surgery or receive opioids often have undiagnosed sleep apnoea. These patients may be at heightened risk of hypoxaemia related complications. This is especially true if they are not monitored during their postoperative care, and if they have pulmonary comorbidity. |
| Patients With Pre-existing Cardiopulmonary Disorders |
Patients with severe cardiopulmonary disorders, who have had at least one episode of documented oxygen, increase and were treated with oxygen, are candidates for monitoring with pulse oximetry. |
| Patients Receiving Conscious Sedation |
Sedation, with or without analagesia, may result in the loss of protective reflexes. The Joint Commission on Accreditation of Healthcare Organizations requires protocols addressing the use of pulse oximetry equipment whenever sedation is provided in a manner that may be reasonably expected to result in the loss of protective reflexes. |
| Neonatal, Paediatric and Elderly Patients |
The typical pulmonary reserve in neonatal, paediatric and elderly patients is often decreased, especially in relation to their increased oxygen demands. These patients may desaturate more quickly than the average adult, increasing their risk for hypoxaemia and related complications. |
| Obstetric Patients | Pain-induced changes in respiration during labour and delivery, and desaturation from epidural morphine or other narcotics following operative delivery, contribute to the risk of hypoxaemia for the obstetric patient. This patient already has diminished pulmonary reserves. |
| The technology - Dependant Patient |
Whether in the inpatient or home care setting, numerous patients depend on technology. Much of this technology enhances optimal oxygenation. Technology-related failures or complications, such as with invasive and non-invasive ventilators and oxygen therapy, may result in hypoxaemia. |
HYPOXAEMIA: THE CLINICAL AND ECONOMIC SIGNIFICANCE
In recent years, numerous clinical studies have discussed the possible role of hypoxaemia with adverse clinical outcomes.
| Hypoxaemia and Wound Healing/Infection |
Oxygen plays an important role in wound healing and infection. Low tissue oxygen levels can compromise wound healing and resistance to infection, leading to prolonged hospital stays and/or healthcare costs. |
| Hypoxaemia and Ischaemia | Postoperative hypoxaemia has been associated with myocardial ischaemia and arrhythmias in patients, both with and without pre-existing cardiac disease. The risk of myocardial ischaemia is related to the degree and duration of hypoxaemia, and may contribute to heart attack and subsequent death. |
| Hypoxaemia and Celebral Function |
Hypoxaemia can impair cerebral function in a number of ways. These include short-term memory loss, confusion, cognitive dysfunction or permanent impairment. In patients with pre-existing circulatory conditions, hypoxaemia can result in cerebral ischaemia or stroke, and subsequent death. |
| Hypoxaemia and Unfavorable Healthcare Costs |
The consequences of hypoxaemia may result in delayed healing and other complications. These can increase the length of stay, rebound to more expensive areas of care, require additional healthcare resources, decrease the functional ability of the patient, and lead to costly malpractice litigation. |
HYPOXAEMIA: TRADITIONAL ASSESSMENT
Although hypoxaemia is a well-recognized safety concern across the health-care continuum, it may present itself in a variety of diverse manners and make assessing patients difficult.
Once traditional method for assessing oxygen is measuring the patient's respiratory rate. However respiratory rate is more often estimated than precise. Additionally, counting respirations has been shown to have virtually no value in detecting hypoxaemia.
Another method of hypoxaemia assessment is evaluating patient skin color. While conventional wisdom holds that if patient skin color changes to a more dusky, bluish or cyanotic tone, the patient is likely hypoxaemic, there are several considerations to keep in mind. Cyanosis is in fact a late sign of hypoxaemia. Cyanosis may not be detected, even in the presence of hypoxaemia, since cyanosis is related to the amount of haemoglobin present in the blood. Patients with severe anaemia may never display signs of cyanosis, despite significant hypoxaemia. Cyanosis is often difficult to detect in patients with certain skin pigments. The cyanosis detection is considered to be subjective at best, and wide observer variability may occur. Therefore, the predictive value of cyanosis for hypoxaemia is poor.
Other assessment parameters, like respiratory effort, mentation and changes in other vital signs, are unreliable indicators of hypoxaemia. Respiratory effort may appear unlabored, even in the presence of hypoxaemia. Although changes in mentation (such as restlessness and confusion) are associated with hypoxaemia, many clinicians don't make the association, and these findings may be attributed to other causes. Changes in other vital signs, including heart rate and ECG, may or may not occur after significant hypoxaemia is present.
These assessment parameters -- including respiratory rate, color, effort, mentation and other vital signs -- usually require the clinician to assess the patient. Even if changes in these parameters result from deteriorating oxygenation status, the clinician is often not present to observe them. Traditional patient assessment activities are usually performed by clinicians when visiting the bedside or home, or at the patient's routine or episodic office visits. Because the oxygenation status of a patient can quickly change, clinicians may not be aware of changes until patient injury or death has occurred. For these reasons, common forms of hypoxaemia detection are inadequate.
Pulse Oximetry
A pulse oximeter is a medical device that provides noninvasive and continuous information about the percent of oxygen that is combined with haemoglobin.
A pulse oximeter is often referred to as a hypoxaemia monitor because it can continuously reflect changes in a patient's arterial oxygen saturation. Monitors are electronic devices intended to keep track of certain situations. Because hypoxaemia can occur at any time and under any clinical circumstance, pulse oximetry is a valuable tool for patient safety and clinical management. A pulse oximeter used to take intermittent measurements of oxygen saturation is more correctly referred to as a "meter," or measuring device. If pulse oximetry is used intermittently, hypoxaemic episodes may be missed.
PULSE OXIMETRY TECHNOLOGY
Pulse oximetry works by applying a sensor to a pulsating arteriolar vascular-bed. The sensor contains a dual light source and photodetector which are used to measure the amount of oxygen that is combined with haemoglobin. The dual light source has a red and an infrared light. These light sources are used because each is absorbed differently by oxyhaemoglobin and deoxyhaemoglobin.
Bone, tissue, pigmentation and venous vessels normally absorb a constant amount of light over time. The arteriolar bed, however pulsates and absorbs variable amounts of light during systole and diastole, as blood volume increases and decreases. The ratio of the amount of each light source absorbed at systole and diastole is translated into an oxygen saturation measurement. An oxygen saturation measurement provided by a pulse oximeter is commonly referred to as SpO2.

ACCURACY
It is important to understand the accuracy level of pulse oximetry measurements. In general, accuracy specifications for pulse oximeters are determined by comparing a saturation obtained from SaO2 and measured by a laboratory co-oximeter (not an arterial blood gas analyzer) with an SpO2 measurement. The SpO2 measurement is taken at the same time arterial blood gas is drawn. This baseline testing is usually performed with healthy adult subjects.
The accuracy specifications for Nellcor® pulse oximeters are usually expressed as "± 2 from 70% to 100% at 1 standard deviation." This means that when the patient's true SaO2 falls within the 70% to 100% range, the Nellcor pulse oximeter will report a saturation that is within 2% of the true saturation about 68% of the time and 4% of the true saturation about 96% of the time.
Below are certain factors that may cause a greater difference between the SpO2 and the SaO2 measured directly from an arterial blood gas.
| Factors | Possible Causes/Rationale | Recommendations |
| Blood Gas Factors | Blood gas is drawn at a different time than the SpO2 measurement is taken. Inaccurate blood gas sampling technique. Blood gas machine is not calibrated accurately. SaO2 is calculated from PaO2 using arterial blood gas analyzer, and not directly measured with laboratory co-oximeter. |
Draw ABG at same time oxygen saturation is measured. Follow proper ABG techniques. Ensure ABG equipment is calibrated. Understand whether SaO2 reports represent measured or calculated Sa02 values. If SaO2 is calculated, do not expect SpO2 value to compare, especially if conditions that cause shifting of the oxyhaemoglobin dissociation curve (such as altered temperature, pH, PaCO2 and 2,3-DPG) are present. |
| Presence of Dysfunctional Haemoglobins | High levels of carboxyhaemoglobin and/or methaemoglobin will cause SaO2 to differ from SpO2 | Suspect elevated dysfunctional haemoglobins if a measured SaO2 differs from SpO2.
Assess oxygenation using a measured SaO2 whenever dysfunctional haemoglobins are suspected. |
| Intracardiac Shunting | Because of abnormal circulatory conditions, such as some forms of congenital heart disease, different oxygen saturation levels may exist in different parts of the body. | If such conditions are present, be aware that SpO2 may differ from SaO2 if measurements are made from different locations. |
| Intravascular Dyes | The injection of intravascular dyes may result in temporary aberration of the SpO2 reading. | Be aware that SaO2 and SpO2 may differ if measurements are made immediately after injection of a dye. |
INNOVATIONS IN TECHNOLOGY: OXISMART AND OXISMART XL

Traditional Pulse oximetry is reliable, especially for immobile and well-perfused patients. However, active patients or those with poor blood flow to a sensor site create challenges for monitoring. Because of motion artifact or because they are weak, pulse signals may be compromised. These conditions may lead to frequent nuisance alarms which can be distracting and time-consuming for clinicians. Because there may be a greater ratio of nuisance alarms to "true" alarms, staff may not respond to every alarm.
Oxismart and Oxismart XL Advanced Signal Processing and Alarm Management are the new generation of pulse oximetry technologies which were developed to address the problem of nuisance alarms common to monitoring conditions of patient motion and low perfusion.

Both Oxismart and Oxismart XL employ signal conditioning to clean the data from the patient. With the newer Oxismart XL, the data is then normailised and whitened to selectively minimalise noise while boosting ture physiologic signals. This whitening process is similar to a stereo systems'sgraphic equalizer, which accentuates some signals and minimizes others. Conditioning enables the Oximeter to perform in low perfusion and high noise environments.
Pattern Match - To determine the pulse rate, Oxismart technolosy utilizes a technology called Pattern Matching, which evaluates the shape of each potential pulse. If the pulse is qualified (i.e. has the right shape) data is sent to the beep tone engine as well as the pulse rate display, and is used to calculate saturation. In this case, pattern matching acts as a gatekeeper for qualifying pulses and passing data through the system. In Oxismart XL technology, pattern matching still drives the beep engine.
However, it is no longer the gatekeeper for the signal datato be sent to the pulse rate or saturation engines, as advanced signal processing technologies for rate and saturation no longer require beat-by-beat recognition. Both Oxismart and Oxismart XL technologies use pattern matching to find the pulse and drive the beep tone. It is the algorithm behind our 'no pulse, no beep' philosophy. The pattern match approach is also well suited to calculating arrhythmic pulses or sudden changes in heart rate, ensuring that during an arrhythmia the Oximeter beeps at the arrhythmic rate. This is the expected behaviour of pulse oximeters in today's market. The Pattern match rate is the proven Oxismart technology which is used to find the pulse, to reliably beep, and to capture arrhythmias and other irregular heart conditions.
Adaptive Comb Filter (ACF) While the strength of pattern matching is to find the pulse, the power of adaptive comb filtering is to reliably track the pulse rate. Similar in concept to digital signal processing use din submarine identification, the ACF cuts through an ocean of non-specific noise to 'lock onto' and follow the pulse at its slowly varying frequency. The algorithm is one of the most important enhancements of Oxismart XL technology.
Best Rate Arbitrator - Oxismart XL technology calculates two pulse rates, one by pattern matching and one by adaptive comb filtering. The best rate arbitrator algorithm chooses the best rate to display, based on proprietary signal quality metrics.
Because a spontaneously moving patient can be assumed to have a pulse, the monitor software continues to search for a pulse as long as continuous motion artifact is detected. If the pulse oximeter fails to detect at least one qualified pulse in a ten-second period, the display will alternate between data and dashes, and a data evaluation period is entered. During this period, if the patient is not moving and has no qualified pulse for six seconds, an audible alarm is triggered and the display flashes zeros. If the patient is constantly moving, the monitor will search for qualified pulses for up to 50 seconds and updates the display each time one is detected. If a qualified pulse signal cannot be detected during this time, an audible alarm sounds and zeros are displayed in the data windows. If an adequate number of qualified pulses are detected, the monitor returns to its normal operating mode and displays updated data on a beat-to-beat basis.
The development of Oxismart technology makes safety monitoring for hypoxemia more reliable and reduces the incidence of nuisance alarms. Clinicians are now better able to identify and manage hypoxemia in any setting where pulse oximetry is used.
In Oxismart XL, three measures are used to ensure that the signal cleaning is accurate and safe. The Kalman C-Lock calculates the saturation value occurring at the pulse rate which is tracked by the ACF. Up to 80 samples per second are used to calculate the ratio of pulsatile red and IR signals through the Least Squares Sat. Finally, the Best Rate Arbitrator chooses the best saturation to display based on the best signal quality.

OXISMART XL
Kalman C-Lock As with the pulse rate engine, saturation is also determined by redundant algorithms. The Kalman C-Lock algorithm calculates the saturation value occurring at the pulse rate that is tracked by the adaptive comb filter. Kalman C-Lock emphasizes signals that are synchronous with the normally rhythmic nature of the pulse signal. This algorithm is a uniquie feature of Oxismart XL technology. Kalman C-Lock can be thought of as a pulse-by-pulse ensemble average of the red and infrared (IR) signals, where the definition of the beginning and end of the pulse comes from the rate (ACF) as opposed to any particular features of the pulse waveform itself. This is similar to the pulse average for some of the earlier generations of Nellcor technology, when ECG triggers are used to define the beginning and the end of a pulse.
Least Squares Sat All pulse oximeters derive their saturation values from a ratio of pulsatile red and IR light signals. Earlier oximeters calculated saturation values using only two data points at the minimum and maximum points on the pulse waveform. With the introduction of Oxsmart technology, up to 80 samples per second are used to calculate the ratio of pulsatile red and IR signals. The oversampling of the waveform requires a calculation method to arrive at the best saturation value. The Least Squares method, which is widely used in statistical calculations, supports the calculation of saturation values in situations of nonrhythmic or rapidly changing pulse rates.
Best Sat Arbitrator Like the arbitrator for pulse rate, the best saturation arbitrator chooses the best saturation to display based on proprietary signal quality metrics.
SAT SECONDS ALARM MANAGEMENT
Nuisance alarms can be caused by two factors: Motion Artefact and Transient Saturation Changes (Episodic Hypoxemia) The exceptional performance of Oxismart XL technology is designed to accurately read saturation through motion. The introduction of SatSeconds Revolutionary Alarm Management gives clinicians for the first time a tool to manage nuisance alarms caused by transient desaturations.
A SatSecond can be thought of as the severity and duration of a Desaturation. It is the product of time and magnitude the patient is outside saturation alarm limits. For example: 1 point either side of the alarm limit for 10 seconds = 10 SatSeconds; 5 points for 20 seconds = 100 SatSeconds.
To manage the nuisance alarms, the clinician may employ the SatSecond feature to trigger an alarm only when the SatSeconds 'clock' reaches a user defined limit of 10, 25, 50 or 100 Sat Seconds. The factory default for this feature is set to 'off'. When three or more violations occur in 60 seconds, an alarm will sound, even if the SatSeconds clock setting has not been reached. This is the SatSeconds 'safety net'.
OPTIMIZING PULSE OXIMETRY
Certain conditions may result in pulse oximetry readings that are unreliable, incorrect or less informative. These considerations and associated recommendations for more reliable monitoring are listed below.
| Consideration | Recommendation |
| Motion | Move sensor to less active site, or replace adhesive. A reflectance sensor may be placed on the forehead, if the patient is not on a ventilator, or is not placed in a Trendelenburg or supine position. Adjust averaging time on pulse oximeter, if possible. Use Oxismart technology to enhance the reliability of measurements during motion. |
| Poor Perfusion | Use an adhesive digit sensor or, if the situations, an ear sensor may be appropriate. Protect sensor site from heat loss or rewarm sensor site as permitted by your clinical policies. Use Oxismart technology to improve the reliability of measurements during poor perfusion. |
| Venous Pulsation | Position digit sensor at heart level. Avoid restrictive taping. Use care when interpreting SpO2 values in patients with elevated venous pressure. |
| Dysfunctional | Dysfunctional haemoglobins, such as carboxy-haemoglobins, Haemoglobins or methaemoglobin, are unable to carry oxygen. However, SpO2 values only report functional saturation - oxygenated haemoglobin as a percentage of functional haemoglobin. Therefore, 5p02 values reported by a pulse oximeter may appear normal when dysfunctional haemoglobins are elevated, although total oxygen content may be compromised due to decreased oxygen carriers. A more complete assessment of oxygenation beyond pulse oximetry is recommended whenever dysfunctional haemoglobins are suspected. |
| Anaemia | Anaemia causes decreased arterial oxygen content by reducing the number of haemoglobin molecules that are available to carry oxygen. Although SpO2 percentages may be in the "normal" range, an anaemic patient may be hypoxic due to reduced haemoglobin levels and therefore reduced total oxygen content. Correcting anaemia can improve arterial oxygen content. The pulse oximeter may fail to provide an SpO2 reading if haemoglobin levels fall below 5 gm/dl. |
| Nail Polish | Remove nail polish (especially brown, blue, green) or apply sensor to unpolished site. |
| Intravascular Dyes | Use care when interpreting SpO2 values after injection of intravascular dyes, which may temporarily affect the reading. |
| Edema | Light from the sensor's light sources may scatter through edematous tissue, although the degree to which this may affect the SpO2 reading is unknown. Position the sensor on non-edematous sites. If peripheral edema is extensive, try the RS-1 5 Nasal Sensor, the Adult Reflectance Sensor, or the D-YSE Ear Clip. |
| Optical Shunt | Optical shunting occurs when some light from the sensor's light sources reaches the photodetector without first passing through the vascular beds. Choose an appropriate sensor for the patient's size, and ensure the sensor remains securely in position with the light sources opposite the photodetector. Replace the sensor when its adhesive is no longer effective. |
| Light Interference | Light interference may result in erratic or inaccurate SpO2 measurements. Cover the sensor with an opaque material in the presence of bright light sources, including direct sunlight, surgical lamps, infrared warming lamps and phototherapy lights. |
| Electrical Interference | Any electrical device, including wall outlets, electrical instruments (such as an electrocautery device), ECG monitors and ventilators, release electrical impulses that may interfere with signal acquisition at the sensor site. This interference can inhibit the pulse oximeter's ability to track the true pulse and result in inaccurate or erratic measurements. Plug the pulse oximeter into a wall outlet that is separate from other devices. Run the sensor cable away from, and perpendicular to, other electrical cables. Shield the sensor site. Newer generation pulse oximetry technology may help minimize electrical interference. |
DETECTION OF HYPOXAEMIA USING PULSE OXIMETRY
Pulse oximetry is a tool that measures arterial oxygen saturation, an important indicator of total arterial oxygen content. Its use as both a safety monitor and clinical management tool has become so significant to patient care that SpO2 is often referred to as the 5th vital sign.

To provide early recognition of hypoxaemia, monitoring with pulse oximetry should be continuous. Spot checks of SpO2 may be used in low-risk patients to verify clinical status and define the potential need for continuous monitoring. Telemetry systems for pulse oximetry allow communication of SpO2 information from the bedside or other remote setting to the caregiver, providing faster identification of changes in oxygen status.
Specific clinical applications for pulse oximetry across the continuum of care include:
- To improve patient safety, clinical management and lower the total cost of care by providing continuous safety monitoring for high-risk patients in any care setting.
- To safely monitor the patient during medical procedures.
- To provide continuous safety monitoring during sedation or pain management.
- When used with telemetry to allow for care of patients in less expensive care settings, especially if they do not require intensive interventions.
- To measure the 5th vital sign in vital signs assessment for patients in any location, including inpatient areas, home and physician offices.
- To determine the need to wean from oxygen therapy, which may result in lowered care costs
- To determine effectiveness of treatments, such as bronchodilators, positioning and suctioning.
- To determine the need for further treatment, such as intubation.
- To assess patient response and tolerance to activities, such as stress testing and activities of daily life.
- To monitor rehabilitation progress.
- To triage patients in the emergency department or clinic.
- To assess admission/transfer/discharge potential of patients.
- To spot check patients for intermittent assessment of oxygenation
Sensor Selection and Use
One of the most critical factors for ensuring reliable pulse oximetry readings is proper sensor selection and application. No single sensor is capable of monitoring all patients under all monitoring conditions. Consider the following when choosing a sensor for your patient:
|

Tyco healthcare offers a wide range of Nellcor adhesive and reusable sensors. The cleaning and care instructions for these are always present in the individual boxes.
Sensor Application
Always apply a sensor according to the Directions for Use. Transmittance sensors must have the light source properly aligned with the photodetector. Reflectance sensors require proper alignment of the sensor against the surface of the skin. Tape is provided with the sensor. Do not apply additional tape to the sensor.
Sensor Site Change
Nellcor reusable sensors should be moved to another site at least every 4 hours to preserve skin integrity. Nellcor adhesive sensor sites should be checked at least every 8 hours. The clinician should document sensor site checks and changes. To protect circulation at the sensor site, use only the adhesive that comes with the sensor. Do not wrap additional tape or other material around the sensor.
Infection Control
Sterile, patient-dedicated sensors offer an infection control advantage over reusable sensors. Reusable sensors require cleaning between patients with 70% alcohol to minimize the risk of cross-contamination. Consider sterile, patient-dedicated sensors for infected patients or those at increased risk for infection, such as neonates or immunosuppressed patients.
Summary of Tips
- Ensure the light sources and photodetector of the sensor are properly aligned, as outlined in the Directions for Use.
- Check adhesive sensor site at least every 8 hours and move to a new site, if necessary. Move reusable sensors to a new site at least every 4 hours.
- Adhesive digit sensors may be reused on the same patient, if the adhesive tape adheres without slipping. Replace the sensor whenever the adhesive quality is depleted. Do not apply additional tape.
- When selecting a sensor site, priority should be given to an extremity that is free from an arterial catheter, blood pressure cuff, or intravascular infusion line.
- Reusable sensors should be thoroughly cleaned between patients. Refer to Directions for Use.
Maintenance and Care
Cleaning the monitor
It is recommended that the following checks be performed every 24 months.
- Inspect the equipment for mechanical and functional damage.
- Inspect the safety relevant labels for legibility.
Caution: Do not spray, pour, or spill any liquid on the monitors, their accessories, switches or openings in the chassis.
For surface-cleaning and disinfecting the monitor, follow your instructions procedures or:
- Surface clean using a soft cloth dampened with a commercial, nonabrasive cleaner or a solution of 70% alcohol in water, and lightly wiping the surfaces of the monitor.
- Monitors may also be disinfected using a soft cloth saturated with a 10% chlorine bleach in tap water solution.
Before attempting to clean an SpO2 sensor, read the directions for use enclosed with the sensor. Each sensor model has cleaning instructions specific to that sensor.
Follow the sensor cleaning and disinfecting procedures in the particular sensor's directions for use.
Returning Monitors
Contact the Nellcor Technical Services Department on 01869 328000, for shipping instructions. It is not necessary to return the sensor or any other accessory items with the monitor, unless instructed by the Technical Services Department. Ensure that the monitor is safely wrapped in a carton for protection during shipment.
Warning: The covers should only be removed by qualified personnel. There are no user-servicable parts inside.
Refer to the operation manual for battery changing procedure. If a service is necessary, contact your local Nellcor representative.
Post Test
- State two ways oxygen is carried in the blood.
- Dissolved in plasma and bound with haemoglobin.
- Dissolved in plasma and bound with carboxyhaemoglobin.
- Bound with haemoglobin and carbon monoxide.
- Dissolved in haemoglobin and bound with plasma.
- Which of the following statements about total oxygen content is true?
- The majority of oxygen carried in the blood is dissolved in the plasma.
- The majority of oxygen carried in the blood is bound with haemoglobin.
- Only 1% to 2 % of oxygen carried in the blood is bound with haemoglobin.
- Total oxygen content is determined by haemoglobin ability to release oxygen to the tissues.
- Which of the following statements about hypoxaemia is false?
- Obstructive sleep apnoea may cause carbon dioxide retention, but not hypoxaemia.
- Certain postoperative patients are at greater risk for hypoxaemia.
- Confusion may be a symptom of hypoxaemia.
- Even the obstetric patient may be at risk for hypoxaemia.
- Pulse oximetry incorporates two technologies that require:
- Red and yellow light.
- Pulsatile blood flow and light transmittance.
- Haemoglobin and methaemoglobin.
- Veins and arteries.
- Which of the following defines "SpO2"?
- Partial pressure of oxygen provided by an arterial blood gas.
- Oxygen saturation provided by an arterial blood gas.
- Oxygen saturation provided by a pulse oximeter.
- Partial pressure of oxygen provided by a pulse oximeter.
- If your patient's oxygen saturation has fallen from 98% to below 90%, after receiving 4 liters 02 via nasal cannula, the following physiologic change may be occurring:
- Oxygen content is rapidly decreasing.
- PaO2 level is rapidly increasing.
- Oxygen content is slowly decreasing.
- PaO2 level is slowly increasing.
- Pulse oximetry can be used to:
- Obtain invasive information about oxygenation.
- Provide acid-base profiles.
- Noninvasively monitor saturation values during ventilator weaning.
- Fully replace arterial blood gas testing.
- Which of the following clinical conditions may contribute to inaccurate oxygen saturation readings as measured by a pulse oximeter?
- Venous pulsations.
- Mild anaemia.
- Sensor placed on a middle finger.
- Monitoring a patient during weaning from oxygen.
- To troubleshoot motion artifact on a finger or toe sensor:
- Ensure the light source is directly across from the photodetector.
- Position the sensor below the level of the heart.
- Cover the sensor with an opaque material.
- Apply additional tape to the sensor to secure it in place.
Post Test Answers
- a
- b
- a
- b
- c
- a
- c
- a
- a
References
- Agency for Healthcare Policy and Research Clinical Practice Guideline. Acute Pain Management: Operative or Medical Procedures or Trauma. Rockville, MD; 1992.
- Chiu L, Eichhorn JH, Hess D, Hoffman L, et al. Principles & Guidelines for Respiratory Monitoring on the General Care Floor. Journal of Clinical Monitoring, 1996;12:411-416.
- Communicore. Hypoxaemia on the General Care Floor: Economic and Risk Management Issues. Newport Beach, CA; 1997.
- Grap MJ. Pulse Oximetry. Aliso Viejo, CA: American Association of Critical Care Nurses Technology Series. Chulay M, Burns 5, Eds. 1996.
- Hoydu CJ. Monitoring Patients Outside the ICU. Advance for Respiratory Care Practitioners. April 1997:13,15.
- Joint Commission on Accreditation of Healthcare Organizations. Revision Calls for Use of Pulse Oximetry Equipment. Perspectives: The Official Joint Commission Newsletter. January/February, 1996.
- Klaas MA, Cheng EY Early Response to Pulse Oximetry Alarms with Telemetry. Journal of Clinical Monitoring. 1994; 10:178-180.
- Kozlowski U, DiMarcello KJ, Stashinko EE, Phifer LC. Pulse Oximeter in a Pediatric Medical-Surgical Population. Journal of Pediatric Nursing. 1994;9: 199-204.
- Mahlmeister MJ. Sensor Selection in Pulse Oximetry. RT: The Journal for Respiratory Care Practitioners. 1998;11:53-59, 113.
- McFadden C, Gutierrez L, Leveque J, Anderson M. CPOM: Alleviating the Demand for ICU Beds. Nursing Management. February 1996;27.
- McGaffigan PA. Hazards of Hypoxemia: How to Protect Your Patient from Low Oxygen Levels. Nursing. 1996;5:41-47.
- Mower WR, Myers G, Nicklin EL, Kearin KT, et al. Pulse Oximetry as a Fifth Vital Sign in Emergency Geriatric Assessment. Academic Emergency Medicine. 1998;5(9):858-870.
- Nellcor Puritan Bennett. Technology Overview: SpO2 Monitors with Oxismart Advanced Signal Processing and Alarm Management Technology. Pleasanton, CA;1998.
- Nyberg L, Gustafson Y, Berggren D, Brannstrom B, et al. Falls Leading to Femoral Neck Fractures in Lucid Older People. Journal of the American Geriatrics Society. 1996;44:156-160.
- Rosenberg J, Pederson MH, Ramsing T, Kehlet H. Circadian Variation in unexpected Postoperative Death. British Journal of Surgery. 1992;79:1300-1302.
- Rosenberg J, Kehlet H. Postoperative Mental Confusion: Association with Postoperative Hypoxaemia. Anesthesiology. 1992;77(suppl):A3 15. Abstract.
- Rosenberg J. Late Postoperative Hypoxemia. Danish Medical Bulletin. February 1995;42:40-46.
- Severinghaus JW, Kelleher, JF. Recent Developments in Pulse Oximetry. Anesthesiology. 1992;76: 1018-1038.
- Sharkey T. Continuous Monitoring Helps Hospitals Cut Costs. Advance for Respiratory Care Practitioners. April 1997:12, 15.
- Smith I. The Economics of Pulse Oximetry. RT. December/January 1995:73-79.
- Trosty S. Hypoxaemia on the General Care Floor: An Emerging Concern for Risk Managers. QRC Advisor. June 1996:12.
- Wojner AW. Widening the Scope: From Case Management to Outcomes Management. The Case Manager. March/April 1997: 77-82.