Depression is a common disorder that can have a debilitating effect on a person's life. It is characterised by persistent sadness, loss of interest or pleasure, feelings of guilt or low self‑worth, disturbed sleep, appetite and libido, tiredness and poor concentration. It is also often accompanied by feelings of hopelessness and suicidal thoughts, and can lead to suicide. Depression can last from weeks to years, and can be recurrent. It can substantially impair an individual's ability to function at work or cope with daily life. Treatments for depression include a range of psychological therapies and antidepressant medications. In severe depression that has not responded to other treatments, electroconvulsive therapy is sometimes applied, which requires anaesthesia, and carries much higher risks than other conventional therapies. Repetitive transcranial magnetic stimulation (rTMS) does not need anaesthesia and can be done on an outpatient basis.
Transcranial magnetic stimulation (TMS) has been used to treat certain disorders, including depression and schizophrenia and to rehabilitate people after stroke. The therapy is particularly encouraging for the use of brain stimulation in chronic disease such as stroke and dementia.
 Transcranial magnetic stimulation (TMS) is a non-invasive method to cause depolarization or hyperpolarisation in the neurons of the brain. TMS uses electromagnetic induction to induce weak electric currents using a rapidly changing magnetic field; this can cause activity in specific or general parts of the brain with minimal discomfort, allowing the functioning and interconnections of the brain to be studied. A variant of TMS, repetitive transcranial magnetic stimulation (rTMS), has been tested as a treatment tool for various neurological and psychiatric disorders including migraines, strokes, Parkinson's disease, dystonia, tinnitus, depression and auditory hallucinations.
Transcranial magnetic stimulation (TMS) is a non-invasive method to cause depolarization or hyperpolarisation in the neurons of the brain. TMS uses electromagnetic induction to induce weak electric currents using a rapidly changing magnetic field; this can cause activity in specific or general parts of the brain with minimal discomfort, allowing the functioning and interconnections of the brain to be studied. A variant of TMS, repetitive transcranial magnetic stimulation (rTMS), has been tested as a treatment tool for various neurological and psychiatric disorders including migraines, strokes, Parkinson's disease, dystonia, tinnitus, depression and auditory hallucinations.
The principle of inductive brain stimulation with eddy currents has been noted since the 20th century. The first successful TMS study was performed in 1985 by Anthony Barker and his colleagues in Sheffield, England. Its earliest application demonstrated conduction of nerve impulses from the motor cortex to the spinal cord, stimulating muscle contractions. The use of magnets rather than a direct electric current to the brain reduced the discomfort of the procedure and research and allowed mapping of the cerebral cortex and its connections.
Effects on the brain
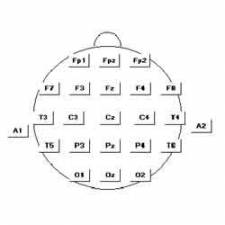
 A purpose‑made electromagnetic coil is held against the scalp with the intention of inducing electric currents in the cerebral cortex. Imaging may be used to help target specific areas of the brain. Treatment is usually considered for patients with depression that has not responded to antidepressant medication or patients for whom antidepressants are not suitable. In rTMS, repetitive pulses of electromagnetic energy are delivered at various frequencies or stimulus intensities. Conventional rTMS is a repetition of individual pulses at a pre‑set interval (train of pulses), whereas theta‑burst rTMS is a repetition of short bursts of pulses at a pre‑set interval (train of bursts). Stimulation can either be delivered unilaterally, over the left or right dorsolateral prefrontal cortex, or bilaterally over both cortices. Bilateral stimulation may be done sequentially or simultaneously.
A purpose‑made electromagnetic coil is held against the scalp with the intention of inducing electric currents in the cerebral cortex. Imaging may be used to help target specific areas of the brain. Treatment is usually considered for patients with depression that has not responded to antidepressant medication or patients for whom antidepressants are not suitable. In rTMS, repetitive pulses of electromagnetic energy are delivered at various frequencies or stimulus intensities. Conventional rTMS is a repetition of individual pulses at a pre‑set interval (train of pulses), whereas theta‑burst rTMS is a repetition of short bursts of pulses at a pre‑set interval (train of bursts). Stimulation can either be delivered unilaterally, over the left or right dorsolateral prefrontal cortex, or bilaterally over both cortices. Bilateral stimulation may be done sequentially or simultaneously.
Treatment with rTMS usually comprises daily sessions lasting about 30 minutes, typically for 2 to 6 weeks.
The effects of TMS can be divided into two types depending on the mode of stimulation:
Single or paired pulse TMS causes neurons in the neocortex under the site of stimulation to depolarize and discharge an action potential. If used in the primary motor cortex, it produces muscle activity referred to as a motor evoked potential (MEP) which can be recorded on electromyography. If used on the occipital cortex, 'phosphenes' (flashes of light) might be perceived by the subject. In most other areas of the cortex, the participant does not consciously experience any effect, but his or her behaviour may be slightly altered (e.g. slower reaction time on a cognitive task), or changes in brain activity may be detected using sensing equipment.
Repetitive TMS produces longer-lasting effects which persist past the initial period of stimulation. rTMS can increase or decrease the excitability of the corticospinal tract depending on the intensity of stimulation, coil orientation and frequency. The mechanism of these effects is not clear although it is widely believed to reflect changes in synaptic efficacy akin to long-term potentiation (LTP) and long-term depression (LTD).
Although TMS is often regarded as safe, the greatest acute risk of TMS is the rare occurrence of induced seizures and syncope. More than 16 cases of TMS-related seizure have been reported in the literature, with at least seven reported before the publication of safety guidelines in 1998, and more than nine reported afterwards. The seizures have been associated with single-pulse and rTMS. Reports have stated that in at least some cases, predisposing factors (medication, brain lesions or genetic susceptibility) may have contributed to the seizure. A review of nine seizures associated with rTMS that had been reported after 1998 stated that four seizures were within the safety parameters, four were outside of those parameters, and one had occurred in a healthy volunteer with no predisposing factors. A 2009 international consensus statement on TMS that contained this review concluded that based on the number of studies, subjects and patients involved with TMS research, the risk of seizure with rTMS is considered very low.
Besides seizures, other risks include fainting, minor pains such as headache or local discomfort, minor cognitive changes and psychiatric symptoms (particularly a low risk of mania in depressed patients). Though other side effects are thought to be possibly associated with TMS (alterations to the endocrine system, altered neurotransmitter and immune system activity) they are considered investigational and lacking substantive proof.
Other adverse effects of TMS are: Discomfort or pain from the stimulation of the scalp and associated nerves and muscles on the overlying skin; this is more common with rTMS than single pulse TMS, Rapid deformation of the TMS coil produces a loud clicking sound which increases with the stimulator intensity that can affect hearing with sufficient exposure, particularly relevant for rTMS (hearing protection may be used to prevent this), rTMS in the presence of incompatible EEG electrodes can result in electrode heating and, in severe cases, skin burns. Non-metallic electrodes are used if concurrent EEG data is required.
The uses of TMS and rTMS can be divided into diagnostic and therapeutic uses.
Diagnosis
TMS can be used clinically to measure activity and function of specific brain circuits in humans. The most robust and widely-accepted use is in measuring the connection between the primary motor cortex and a muscle to evaluate damage from strokes, spinal cord injuries, multiple sclerosis and motor neuron disease. TMS has been suggested as a means of assessing short-interval intracortical inhibition (SICI) which measures the internal pathways of the motor cortex but this use has not yet been validated.
Therapy
Studies of the use of TMS and rTMS to treat neurological and psychiatric conditions have shown only modest effects with little confirmation of results. However, publications reporting the results of reviews and statistical meta-analyses of earlier investigations have stated that rTMS appeared to be effective in the treatment of certain types of major depression under certain specific conditions. rTMS devices are marketed for the treatment of such disorders in Canada, Australia, New Zealand, the European Union, Israel and the United States.
A recent meta-analysis of 34 studies comparing rTMS to sham treatment showed an effect size of 0.55 (p <.001). This is comparable to commonly reported effect sizes of pharmacotherapeutic strategies for treatment of depression in the range of 0.17-0.46. However, that same meta-analysis found that rTMS was significantly worse than electroconvulsive therapy (effect size -0.47), although side effects were significantly better with rTMS. An analysis of one of the studies included in the meta-analysis showed that one extra remission from depression occurs for every 3 patients given electroconvulsive therapy rather than rTMS (number needed to treat 2.36).
There is evidence that rTMS can temporarily reduce chronic pain and change pain-related brain and nerve activity, and TMS has been used to predict the success of surgically implanted electrical brain stimulation for the treatment of pain.
Other areas of research include the rehabilitation of aphasia and motor disability after stroke, tinnitus, Parkinson's disease and the negative symptoms of schizophrenia. TMS has failed to show effectiveness for the treatment of brain death, coma, and other persistent vegetative states.
It is difficult to establish a convincing form of "sham" TMS to test for placebo effects during controlled trials in conscious individuals, due to the neck pain, headache and twitching in the scalp or upper face associated with the intervention. "Sham" TMS manipulations can affect cerebral glucose metabolism and MEPs, which may confound results. This problem is exacerbated when using subjective measures of improvement. Depending on the research question asked and the experimental design, matching this discomfort to distinguish true effects from placebo can be an important and challenging issue.
A recent multicenter trial of rTMS in depression used a "sham" placebo treatment that appeared to mimic the sound and scalp stimulation associated with active TMS treatment. The investigators concluded: "Although the treatment effect was statistically significant on a clinically meaningful variable (remission), the overall number of remitters and responders was less than one would like with a treatment that requires daily intervention for 3 weeks or more, even with a benign adverse effect profile". However, a review of the trial's report has questioned the adequacy of the placebo, noting that 'treaters' were able to guess whether patients were receiving treatment with active or sham TMS, better than chance.
 TMS - Butterfly Coils TMS uses electromagnetic induction to generate an electric current across the scalp and skull without physical contact. A plastic-enclosed coil of wire is held next to the skull and when activated, produces a magnetic field oriented orthogonally to the plane of the coil. The magnetic field passes unimpeded through the skin and skull, inducing an oppositely directed current in the brain that activates nearby nerve cells in much the same way as currents applied directly to the cortical surface.
TMS - Butterfly Coils TMS uses electromagnetic induction to generate an electric current across the scalp and skull without physical contact. A plastic-enclosed coil of wire is held next to the skull and when activated, produces a magnetic field oriented orthogonally to the plane of the coil. The magnetic field passes unimpeded through the skin and skull, inducing an oppositely directed current in the brain that activates nearby nerve cells in much the same way as currents applied directly to the cortical surface.
The path of this current is difficult to model because the brain is irregularly shaped and electricity and magnetism are not conducted uniformly throughout its tissues. The magnetic field is about the same strength as an MRI, and the pulse generally reaches no more than 5 centimetres into the brain.
Coil types
The design of transcranial magnetic stimulation coils used in either treatment or diagnostic/experimental studies may differ in a variety of ways. These differences should be considered in the interpretation of any study result, and the type of coil used should be specified in the study methods for any published reports.
The most important considerations include: The type of material used to construct the core of the coil The geometry of the coil configuration The biophysical characteristics of the pulse produced by the coil.
With regard to coil composition, the core material may be either a magnetically inert substrate (i.e., the so-called 'air-core'coil design), or possess a solid, ferromagnetically active material (i.e., the so-called 'solid-core' design). Solid core coil design result in a more efficient transfer of electrical energy into a magnetic field, with a substantially reduced amount of energy dissipated as heat, and so can be operated under more aggressive duty cycles often mandated in therapeutic protocols, without treatment interruption due to heat accumulation, or the use of an accessory method of cooling the coil during operation. Varying the geometric shape of the coil itself may also result in variations in the focality, shape, and depth of cortical penetration of the magnetic field. Differences in the coil substance as well as the electronic operation of the power supply to the coil may also result in variations in the biophysical characteristics of the resulting magnetic pulse (e.g., width or duration of the magnetic field pulse). All of these features should be considered when comparing results obtained from different studies, with respect to both safety and efficacy.
A number of different types of coils exist, each of which produce different magnetic field patterns. Some examples: round coil: the original type of TMS coil figure-eight coil (i.e. butterfly coil): results in a more focal pattern of activation double-cone coil: conforms to shape of head, useful for deeper stimulation four-leaf coil: for focal stimulation of peripheral nerves.
Design variations in the shape of the TMS coils allow much deeper penetration of the brain than the standard depth of 1.5 cm. Circular, H-shaped, double cone coils and other experimental variations can induce excitation or inhibition of neurons deeper in the brain including activation of motor neurons for the cerebellum, legs and pelvic floor. Though able to penetrate deeper in the brain, they are less able to produce a focused, localized response and are relatively non-focal.
To look at the effect of TMS on growth of neurons, Dr Fortunato Battaglia and Dr Hoau-Yan Wang at City University in New York, gave mice the therapy for five days and then examined their brains, New Scientist magazine reported. They found large increases in the proliferation of stem cells - immature cells that go on to develop into nerves and other kinds of tissue - in a part of the brain called the dentate gyrus hippocampus. These cells divide throughout life and are believed to play a crucial role in memory and mood regulation. In particular they found one receptor in the cells was activated. A subsequent study which is due to be published shortly showed that the activity of this receptor declines in mice and humans with Alzheimer's disease.
Brain recovery
Taking the two studies together, Dr Battaglia said there were important implications for neurorehabilitation. "When you have a stroke there is an area that is damaged and there are several ways your brain can recover. "One is that the area which is not damaged will have to work more and it's that we can promote with brain stimulation."
He added that the hippocampus is much deeper in the brains of humans so it would be important to make sure the technique could produce the same effect as in mice. "But it might improve symptoms or delay progression of things like Alzheimer's disease," he added. Professor Vincent Walsh from the Institute of Cognitive Neuroscience at University College London said the findings were a good first step. "There are lots of examples of TMS enhancing function in some way but we have never been able to explain the mechanics of how it might work. "The work is particularly encouraging for the use of brain stimulation in chronic disease such as stroke and dementia. "The challenge now is to find ways of combining stimulation with drug therapies."
Trancranial stimulation for Migraine
Migraines are severe headaches that are usually accompanied by additional symptoms including nausea and vomiting, and aversion to light and sound. A migraine may or may not be preceded by a warning “aura” where the person may experience visual changes such as seeing flashing lights or zigzag lines or other symptoms. The cause of migraines is not known, but involves sudden contraction and then dilation of blood vessels in the brain. Numerous triggers have been identified including changes in hormone levels, environment (such as bright lights), diet and emotions. Transcranial magnetic stimulation (TMS) has been evaluated by the National Institute for Clinical Excellence (NICE) for use during the aura before a migraine episode or at the start of a migraine episode, with the intention of stopping or reducing the severity of the episode ('treatment'); or at planned intervals, with the intention of reducing the frequency and/or severity of migraine episodes ('prevention').
 This TMS treatment involves the person holding a device on their scalp that then delivers a magnetic pulse through the skin. The device is portable and can be used at home or wherever is convenient. The number of pulses can be changed – from a single pulse (sTMS) to repeated pulses (rTMS). The strength, frequency and length of time it is given can also be varied for each individual. The device records the treatments, which can be useful as part of a headache diary. NICE reports that TMS can be used in people who experience migraine with or without aura. It is not fully understood why delivering TMS can reduce the severity or frequency of migraines in some people. Many media reports talk of the pulses “short-circuiting” the “electrical storms” of a migraine. Such terms are fanciful and unhelpful. All we can say with certainty is that we know that some people with migraines find TMS helpful. It is unclear why this is the case.
This TMS treatment involves the person holding a device on their scalp that then delivers a magnetic pulse through the skin. The device is portable and can be used at home or wherever is convenient. The number of pulses can be changed – from a single pulse (sTMS) to repeated pulses (rTMS). The strength, frequency and length of time it is given can also be varied for each individual. The device records the treatments, which can be useful as part of a headache diary. NICE reports that TMS can be used in people who experience migraine with or without aura. It is not fully understood why delivering TMS can reduce the severity or frequency of migraines in some people. Many media reports talk of the pulses “short-circuiting” the “electrical storms” of a migraine. Such terms are fanciful and unhelpful. All we can say with certainty is that we know that some people with migraines find TMS helpful. It is unclear why this is the case.
TMS is not a cure for migraine. Evidence from clinical trials has shown that it can reduce the severity or frequency of attacks in some people, but may not be effective for others. In a multicentre randomised controlled trial of TMS in 164 people who had migraine with aura:
- 39% of the patients were pain-free two hours after stimulation compared with 22% of patients using a placebo (control)
- 29% were still pain-free after 24 hours with no recurrence of migraine or need for medication, compared with 16% using placebo
This therapeutic transcranial magnetic stimulation (TMS) device was found to be significantly more effective than placebo control in treating migraine with aura. The trial studied the use of the eNeura TMS device for patient-administered home treatment of migraine with aura. In the trial, 201 patients from 18 centres suffering from migraine headaches were asked to use the device at the onset of their aura; 102 received an active TMS device, and 99 were given an identical-appearing, non-active or “sham" device that did not deliver a magnetic pulse. Patients were instructed to administer two single pulses of TMS. Each pulse is delivered in one millisecond, or 1/1000 of a second.
Patients recorded migraine pain intensity and symptoms using an electronic diary. Analysis of the primary end point revealed 39% using the TMS treatment system were pain-free at two hours after treatment, as compared to 22% of those using the "sham" device. With a p-value of 0.018 and a therapeutic gain of 17%, these results are both statistically significant and clinically meaningful.
The UK National Institute of clinical Excellence (NICE) states:
‘The evidence on repetitive transcranial magnetic stimulation for depression shows no major safety concerns. The evidence on its efficacy in the short‑term is adequate, although the clinical response is variable. Repetitive transcranial magnetic stimulation for depression may be used with normal arrangements for clinical governance and audit’.
Sources:
http://news.bbc.co.uk/1/hi/health/6683757.stm
http://en.wikipedia.org/wiki/Transcranial_magnetic_stimulation
http://www.bbc.co.uk/news/uk-northern-ireland-14823424
http://news.sky.com/story/1198892/migraines-magnetic-device-offers-pain-relief
http://www.dailymail.co.uk/health/article-2543388/Migraine-hope-gadget-blasts-pain-away-approved.html
https://www.brainclinics.com/repetitive-transcranial-magnetic-stimulation-rtms
http://publications.nice.org.uk/transcranial-magnetic-stimulation-for-treating-and-preventing-migraine-ipg477
Edited by John Sandham.