Acceptance testing is a critical stage in the lifecycle of any medical device, ensuring that new, repaired, or loaned equipment is safe, functional, and meets specified performance criteria before it's put into service. This rigorous process safeguards patients, protects staff, and ensures compliance with legal and clinical governance requirements. The Electronic and Biomedical Engineering (EBME) department plays a crucial role in establishing and overseeing these processes, checking that equipment meets safety standards, clinical requirements, and the hospital's procurement needs from the day it arrives.
In the UK, the Medicines and Healthcare products Regulatory Agency (MHRA) plays a central role in overseeing medical device regulation, with significant legislative updates occurring and planned for 2025 and beyond.
The Evolving Regulatory Environment in the UK
The UK's medical device regulatory landscape is dynamic, especially in the post-Brexit era. While previously aligned with EU Directives (MDD, AIMDD, IVDD), the UK is progressively developing its own framework. Key updates and upcoming changes include:
- UK Medical Devices Regulations (UK MDR 2002): These remain the foundational regulations for placing devices on the Great Britain market. However, there are transitional arrangements that allow CE-marked devices (compliant with EU MDD, AIMDD, MDR, or IVDR) to be placed on the GB market, generally until June 2028 or June 2030, depending on the device type and certification.
- New UK Regulatory Framework (under development): The UK government, through the MHRA, is actively implementing a new, strengthened regulatory framework:
- Post-Market Surveillance (PMS) Regulations: Coming into force in June 2025, these regulations significantly enhance requirements for manufacturers to monitor devices once on the market. This includes stricter data collection, shorter timelines for serious incident reporting, and more rigorous periodic reviews of PMS data, especially for implantable devices. This aims to improve traceability of incidents and facilitate earlier detection of safety issues.
- Pre-Market Requirements: Statutory Instruments expected in 2025 and 2026 will introduce new pre-market requirements, including:
- Increased classification for certain medical devices, leading to greater scrutiny.
- A legal requirement for Unique Device Identification (UDI) to enhance traceability.
- A requirement for manufacturers of implantable medical devices to provide 'implant cards' to patients.
- New rules on public claims about devices.
- A framework for international recognition, enabling swifter access for devices approved by comparable regulators (e.g., in Australia, Canada, EU, USA).
- Updates to essential requirements for medical devices to align more closely with EU MDR, including cybersecurity requirements for software as a medical device (SaMD) and AI.
- Care Quality Commission (CQC) Regulations: The CQC continues to scrutinise healthcare providers to ensure equipment is suitable, properly maintained, and used safely, linking directly to acceptance testing and ongoing management.
- CQC Regulation 15: Safety, availability and suitability of equipment states that "The registered person must make suitable arrangements to protect service users and others who may be at risk from the use of unsafe equipment by ensuring that equipment provided for the purposes of the carrying on of a regulated activity is—properly maintained and suitable for its purpose; and used correctly." It also mandates that equipment must be "available in sufficient quantities" and, where provided for daily living, "promotes the independence and comfort of service users." This highlights the direct link between acceptance testing and meeting CQC compliance.
The Importance of Modern Acceptance Testing
Given the evolving regulatory landscape and technological advancements, acceptance testing is more critical than ever. It serves multiple purposes:
- Patient and Staff Safety: Verifies that the device is free from defects, functions as intended, and poses no undue risk.
- Regulatory Compliance: Ensures adherence to MHRA regulations, CQC standards, and other relevant national guidelines.
- Performance Verification: Confirms that the equipment meets manufacturer specifications and is suitable for its intended clinical purpose.
- Asset Management: Integrates new equipment into the healthcare organisation's inventory, facilitating effective lifecycle management, maintenance scheduling, and eventual disposal.
- Financial Stewardship: Prevents the deployment of faulty equipment, reducing potential costs associated with repairs, downtime, and adverse incidents.
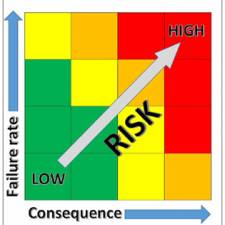
- Risk Mitigation: Identifies and addresses potential risks early in the equipment's life.
Key Elements of Modern Acceptance Testing
While core principles remain, the process has become more sophisticated, requiring detailed checks and meticulous record-keeping. With every device, individual checks should be recorded as 'Pass', 'Fail', or 'N/A' (not applicable). Any minor failures that can be easily rectified must be recorded, along with any remarks and corrective actions.
1. Records and Documentation
The first task is to ensure comprehensive records are taken that can be entered into the equipment management database once the acceptance testing is completed. Essential details include:
- Generic Equipment Type: e.g., 'Defibrillator'.
- Equipment Number: From (or to be entered into) the equipment database.
- Model of the Device: As shown on the manufacturer's label.
- Job Number: Allocated from the database for this acceptance test.
- Accessories: A list of all accessories delivered with the device, which must be checked.
- Order Number: For cross-reference with the supplier.
- Serial Number: Unique identifier for the device.
- Cost: The cost of the device with accessories.
- Manufacturer and Supplier: Names and contact details (if different).
- Date of Acceptance: Into the hospital.
- Warranty Expiry Date.
- Technician's Signature: Who carried out the acceptance testing.
- Location of Technical Documents: Both physical and digital copies.
- Location of the Equipment: (Ward or Department).
- Departmental Equipment Controller: Person within the ward or department responsible for that device.
2. Acceptance Checks
2.1 General Considerations
- Packaging Inspection: Check for transit damage.
- Intact Delivery: Verify the equipment arrived as specified in the order, with correct accessories and documentation.
- Documentation: User manuals are crucial, and it's good practice to request them in PDF format to allow placement on the Hospital intranet for easy access by all users. This also supports initiatives for paperless operations.
- Completeness and Undamaged State: Ensure the equipment is complete and undamaged upon removal from packaging. All control knobs, fuses, etc., should be intact.
- Chemicals/Liquids: If applicable, inspect any contained chemicals or liquids for correctness.
- Mobility: If the device has wheels or castors, ensure they roll freely and brakes work effectively.
- Labelling: Inspect all labelling for correct language and compliance. All medical devices should carry a UKCA mark (or a valid CE mark under transitional arrangements) indicating compliance with relevant regulations.
2.2 Electrical Safety Markings
- Device Labels: Identify and record the electrical safety markings, such as Class I or II, and Type B, BF, CF, AP, or APG. Record these on the acceptance form and in the database.
- Current Regulations: Be aware of the current electrical safety regulations specific to the device being tested (e.g., IEC 60601-1 and its national amendments).
2.3 Mains Connection Inspection
- Cable and Plug Condition: Pay attention to the condition and type of power cable and plug.
- Plug Terminal Connections: Ensure they are terminated properly with the correct cable colour code and that the cord grip is attached.
- Fuses: Verify fuses are correct and in accordance with the rating stated on the device or in the technical documentation.
- Equipment Protection: Confirm protection is in accordance with current requirements (e.g., special interlocking electrical supply sockets for some laser equipment).
- Voltage Settings: Check that voltages are set to the correct value for the mains supply.
- Earth Terminal Symbol: Verify it is correct if applicable to the device.
2.4 Electrical Safety Measurements
Once the equipment classification and type have been determined, ensure the device meets safety requirements by carrying out electrical measurements. These are typically performed using an automated electrical safety analyzer and determine a pass or fail for:
- Earthing of the Equipment:
- Earthing of Accessories:
- Insulation Resistance:
- Earth Leakage Current:
- Enclosure Leakage Current:
- Patient Leakage Current: Where applicable to the device.
2.5 Installation and Operational Tests
- Functional Verification: Ensure the equipment functions correctly as per manufacturer specifications. This should involve tests carried out by the user or the supplier.
- User Training: Once the equipment user has received adequate training to use the device safely, they should then verify that the device is operating correctly in the clinical environment and inform the technician once they are satisfied.
2.6 Ancillary Connections and Environment
- Other Services: Inspect connections for gas, water, vacuum, etc., to ensure compatibility.
- Controlled Environment: If the user manual indicates a need for a controlled environment for correct operation, verify these conditions are met.
- Device Controls: All actual device controls, indicators, alarms, and emergency stop functions must be verified before formal acceptance (where applicable).
Emerging Technologies and Their Impact on Acceptance Testing
The rapid pace of technological innovation necessitates adapting acceptance testing protocols:
- Artificial Intelligence (AI) and Machine Learning (ML): AI-powered medical devices require new approaches to validation, focusing on the integrity of algorithms, data biases, and the explainability of AI decisions. Testing must ensure AI systems function reliably and safely within clinical contexts.
- Wearable Devices and Remote Monitoring: The proliferation of these devices demands testing for connectivity, data accuracy, cybersecurity, and integration with broader healthcare systems.
- Internet of Medical Things (IoMT): Devices connected to networks introduce complex cybersecurity risks. Acceptance testing must include robust vulnerability assessments and network security checks.
- 3D Printing: Acceptance testing may need to verify the integrity and biocompatibility of 3D-printed components in certain medical devices or custom-made devices.
- Telehealth and Virtual Care Platforms: These platforms facilitate the use of medical devices remotely. Their integration requires assurance of secure data transmission and appropriate functional validation in a virtual environment.
- Automated Testing and Predictive Analytics: New tools are emerging that can automate parts of the testing process, improving efficiency and consistency. AI-powered analytics can also aid in predictive maintenance and failure analysis, informing future testing protocols.
Formal Acceptance and Further Action
Once all regulatory and operational criteria for acceptance have been satisfied, the device can be labelled with an asset number and tested label. It is then formally handed over to the user. After acceptance, the supplier and internal supplies department should be informed, and the equipment formally released to the clinical user.
- Modifications: If modifications are necessary to ensure the device will pass acceptance, the supplier (as agreed by the hospital) should make these. The modification must then be re-checked for compliance.
- Rejection and Quarantine: If any serious shortcomings remain after testing, the device should be rejected and quarantined.
- MHRA Notification: If the defect is thought to be of a manufacturing nature or poses a significant safety risk, it may be necessary to inform the Medicines and Healthcare products Regulatory Agency (MHRA).
Acceptance testing of medical equipment is a dynamic and essential process that must continuously adapt to regulatory changes and technological advancements. The focus remains firmly on patient safety, underpinned by rigorous testing, comprehensive documentation, and a thorough understanding of the evolving UK regulatory framework. Biomedical engineering departments (EBME) and healthcare organisations must prioritise ongoing training for their staff, invest in appropriate testing equipment, and foster strong collaboration with clinical users and manufacturers to ensure that all medical devices are safe, effective, and compliant throughout their operational life. Embracing new technologies and continually refining acceptance testing protocols will be crucial for delivering high-quality and safe patient care in the years to come.