On the 3rd February 2023, the UK government released a policy paper entitled ‘Medical technology strategy’. The paper discusses the role of medical technology in improving health outcomes and the size of the medtech sector in the UK.
The Government Vision for Medical technology focusses on 3 central objectives:
- Right product
- Right price
- Right place

Medical technology is an evolving domain, with scientific and engineering breakthroughs prompting new innovations and changing societal needs provoking creative approaches. It can be found in hospitals, ambulances, doctors' surgeries and even our own homes and play a crucial role in the whole pathway of care, supporting people from prevention, through to diagnosis, treatment and ongoing management of health. Effective use of medical technology will be critical in moving forward, and supporting the elective recovery plan by reducing diagnostic bottlenecks and waiting lists, and by delivering new and improved ways to treat and support patients.
Medical technology can reduce health disparities by improving the assessment of health risks and help us to better manage long-term conditions, supporting people to live longer, healthier, more independent lives. Innovations in medical technology will also support the NHS in delivering its net zero ambition in a variety of ways, from using materials more efficiently to the introduction of more sustainable models of care. As a significant area of spend, medical technology also has an important role to play in the long-term financial sustainability of the UK health and care system.
Will Quince - Minister of State (Minister for Health and Secondary Care)
 “As we set out on this journey, I would like to extend my thanks to our colleagues across the health and care system, the medical technology industry and devolved administrations for their valuable input. We have been exceptionally fortunate during the development of this strategy to be able to engage and collaborate with a wide range of people and organisations to help us build a broad and balanced picture of how we can drive the sector forwards, and I am confident this strategy, and the continued collaborative effort behind it, will deliver tangible benefits across the UK as a whole for patients and care providers as well as the UK medical technology industry and those working in the sector.”
“As we set out on this journey, I would like to extend my thanks to our colleagues across the health and care system, the medical technology industry and devolved administrations for their valuable input. We have been exceptionally fortunate during the development of this strategy to be able to engage and collaborate with a wide range of people and organisations to help us build a broad and balanced picture of how we can drive the sector forwards, and I am confident this strategy, and the continued collaborative effort behind it, will deliver tangible benefits across the UK as a whole for patients and care providers as well as the UK medical technology industry and those working in the sector.”
This strategy is intended to ensure the health and social care system can reliably access safe, effective and innovative medical technologies that support the continued delivery of high-quality care, outstanding patient safety and excellent patient outcomes in a way that makes the best use of taxpayer money.
The NHS alone spends an estimated £10 billion a year on medtech (DHSC Estimate, 2021, based on multiple data sources). The medtech sector is an important provider of opportunities for jobs and development of specialist skills in local areas across the UK.

The governments medtech strategy aspires to deliver the following actions:
- The Medtech Directorate will set up the appropriate governance structures to achieve the aims set out in the strategy
- The DHSC Director for Medtech will oversee the governance, implementation, and ongoing activities in the sector
- The government will work with stakeholders to develop an implementation plan
Net zero - The medtech strategy will support sustainability and meeting the NHS net zero target. The strategy outlines the need to find clinically safe and effective products that are better for the environment through reuse and remanufacture.
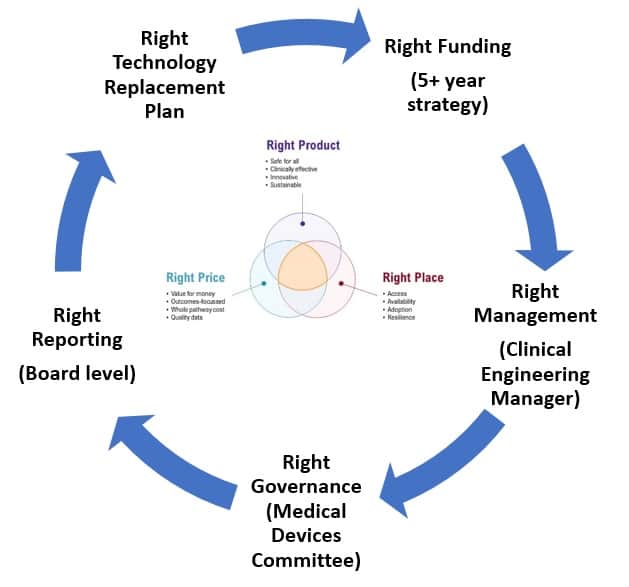
To have the right product in the right place at the right time also requires the right funding, the right management, the right monitoring, and the right reporting. Whether this is a government led strategy, or local NHS organisation strategy, the same rules apply.
Any healthcare organisations that wants to implement improvements that are intended to impact on clinical outcomes must first understand the importance of creating a strategic technology plan based on the current and future business of their organisations.
These plans can be developed quickly in organisations that have accurate data such as:
- How many assets do you have?
- How many do you need to deliver the clinical outcomes / business of the organisation?
- What are your utilisation rates for current technology?
- Do you need more, less, or different technology?
- Are your devices maintained?
- Is reliability and safety assured?
- Are you compliant with current regulations? (Internal audits)
- Does your data inform your strategy?
The current NHS ‘make-do and mend’ methods – repairing outdated equipment, and buying Healthcare technology ‘as required’ in an attempt to save money actually leads to less standardisation, significant age variances (within similar asset groups) making equipment replacement planning difficult. Ultimately this outdated approach leads to higher costs, higher risks to patients, and inefficiencies.
The National Patient Safety Agency recognises that NHS equipment is very poorly utilized with many devices lying idle. Improving utilization of technology can reduce the volume of assets needed and thereby reduce costs by up to 30%, resulting in a significant reduction in the investment required to replace devices and software. If NHS Trusts improve their technology management, they can successfully improve clinical outcomes, improve patient throughput, and reduce their costs.NHS technology management may include areas such as: Procurement (equipment replacement planning), consumables management, service delivery, decontamination, equipment library, user training, telehealth platforms (with 24 Hour Call Centre support), thus providing a complete technology platform for a busy NHS Trust.
The key objectives for healthcare technology management are the following:
- Financing and managing equipment replacements
- Current and future cost management
- Reducing overall costs
- Reliable equipment replacement forecasting
- Optimisation of cash flow
- Improving the patient care experience
- Increase patient safety through standardisation
- Reduce unnecessary hospitalization through home warding (Telehealth)
The risks of organisations not having the right product in the right place at the right time:
- Patients may die or be seriously harmed
- Longer bed stays / bed management problems
- Higher costs for capital purchase
- Higher costs for revenue purchases
- Higher costs for externally contracted maintenance
- Higher legal fees (Clinical negligence)
- Higher insurance costs
- Failure to meet CQC regulations
Senior politicians and NHS Executives accept that healthcare technology can assist with transformational improvements for the NHS. The improvements will deliver higher productivity, safer care, and substantial cost savings. To enable technology to deliver transformational changes requires the government to not only inject capital, but also to have an approach that is inclusive of NHS stakeholders (Clinicians, nurses, scientists, engineers, and managers, etc). These stakeholders hold the knowledge required to jointly deliver a transformational technological solution but unfortunately, although there is momentum, we must ensure that the processes and policies that guide the transformation are properly thought through.
The NHS has an ageing fleet of portable and fixed assets. It is imperative to consider the impact that modern medical equipment can have on reducing the amount of administration that nurses, doctors, and other stakeholders spend inputting data manually. Modern devices are capable of automatically inputting data from portable and fixed devices into medical records without the need for manual data entry. This requires investment in new medical technology and implementation of new ways of working. As Dr Peter Melton - Co-Chair NHS Commissioning Assembly said: “Technology alone can’t deliver transformation in care, but when embedded in a wider package of care and new ways of working, the combined innovation can have a powerful impact on improving patient outcomes and reducing inequality.”


