Senior politicians and NHS Executives accept that healthcare technology can assist with transformational improvements for the NHS. The improvements will deliver higher productivity, safer care and substantial cost savings. To enable technology to deliver transformational changes requires the government to not only inject capital, but also to have an approach that is inclusive of NHS stakeholders (Clinicians, nurses, scientists, engineers, and managers, etc). These stakeholders hold the knowledge required to jointly deliver a transformational technological solution but unfortunately, although there is momentum, we must ensure that the processes and policies that guide the transformation are properly thought through. Although senior politicians and NHS executives are focussing on technology to deliver transformational improvements, there is a concern that portable and fixed assets (that are used by stakeholders) have not been properly considered as part of this technological transformation.
At present, the NHS has an ageing fleet of portable and fixed assets which do not connect with any IT systems. It is imperative to consider the impact that modern medical equipment (with Bluetooth and Wi-Fi connectivity) can have on reducing the amount of administration that nurses, doctors, and other stakeholders spend inputting data manually. Modern devices are capable of automatically inputting data from portable and fixed devices into medical records without the need for manual data entry. This requires investment in new medical technology and implementation of new ways of working. As Dr Peter Melton - Co-Chair NHS Commissioning Assembly said: “Technology alone can’t deliver a transformation in care, but when embedded in a wider package of care and new ways of working, the combined innovation can have a powerful impact on improving patient outcomes and reducing inequality.” (NHS Commissioning Assembly, 2015)
The NHS spends approximately £4.6billion of its budget on equipment and consumables. (NHS Protect, 2015). For 2015/16, the overall NHS budget was £116.4 billion. This equates to a 3.9% spend on healthcare technology and consumables. Although technology spend is relatively small (in comparison with overall NHS spend) there is still pressure from NHS executives to avoid investment in new medical equipment thus attempting to reduce the £4.6 billion that is currently being spent. This goes against the rhetoric coming from senior politicians about using technology to trigger process change.
Figure 1: Technology spend

Poorly implemented technology projects can lead to higher risks and higher costs
Although it is recognised that well managed adoption of new technology within the NHS can deliver safer more efficient care of patients, in many NHS Trusts, new technology adoption is poorly thought through and poorly implemented leading to further risks and higher costs. As recognised by the NHS Institute as far back as 2007: ‘The danger with technology-enabled improvements is that the people and process aspects are overlooked in the enthusiasm to get the kit up and running’. (NHS Institute for Innovation and Improvement, 2007). It is vital when delivering a Technology Strategy that the solution is designed with involvement of all stakeholder groups (Staff and patients), the technology reputation and specification, and the process itself. The links between stakeholders, processes and technology must be carefully considered to properly understand the interdependency of all three elements in any improvement process:

When considering the connections between stakeholders, processes and technology, we must analyse any processes that might need to change, and what technologies will help us make that change. Also, people’s roles often change as a result of the new technology, so it is imperative to consider the impact on stakeholders, and involve them in making the changes. Ultimately, how are patients and staff likely to feel about the changes and the technology - and what needs to happen to support them? This is especially important when looking at introducing step-down care options such as hospital hotels or acute home warding.
Hospital Hotels – Developing step down care facilities The NHS is currently being challenged by Lord Carter to develop operating models for step down care. Innovative models are being proposed such as hospital hotels.
The NHS is currently being challenged by Lord Carter to develop operating models for step down care. Innovative models are being proposed such as hospital hotels.
The hospital hotel concept is not new but also not yet well established or developed within the UK. This concept was first developed as Patient Hotels in Sweden in 1988 to meet increasing demand but within a restricted budget. The concept in Sweden was based on a radical re-think of the healthcare delivery model and the introduction of a graduated care model where appropriate sub-acute patients were transferred to the hotel. The concept was based on a philosophy of re-enablement and engaging the family where this was possible. The model has been successfully duplicated within other locations in Scandinavia, but has not been developed in the UK, potentially because of concerns of patient deterioration or re-admission. These concerns can now be addressed using technology that is Bluetooth and wireless enabled.
Figure 2: Technology solutions to treat more patients per day

Devices are becoming much simpler to use, to the point where patients can now take their own observations such as: Oxygen saturation, pulse rate, blood pressure, spirometry, respiration rate, blood sugar, weight, temperature, etc. using wifi or Bluetooth devices that automatically ‘push’ the data into the patient record allowing doctors and nurses to view the patient data from their PC, tablet, or phone.
Figure 3: Connectivity of technology
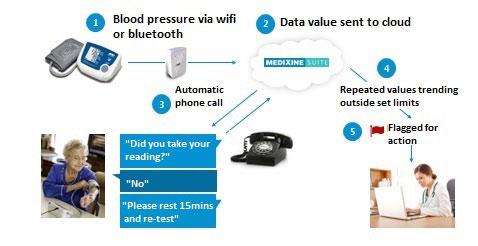
Doctors and nurses can follow the condition of their patients, even though they are in the hospital hotel or at home. This connectivity allows them the comfort to step them down into the hospital hotel, or even to their homes (subject to them being able to care for themselves or have support from family or friends). In summary the hospital hotel model offers the NHS an opportunity to meet the challenges of improving patient experience and the quality of care whilst reducing costs at the same time.
When implementing new healthcare technology processes, it is important to consider how new technology fits with existing systems. Opportunities are wasted when implementing new IT systems if they do not communicate with other systems and devices. Therefore, NHS executives must ensure adequate planning has gone into specifying, setting up, and testing that different technologies do actually ‘talk’ to each other thus leading to improved productivity. As with any healthcare technology, user training is imperative if technology is to be used safely and effectively. Finally, data security issues need to be addressed ensuring patient information is secure.
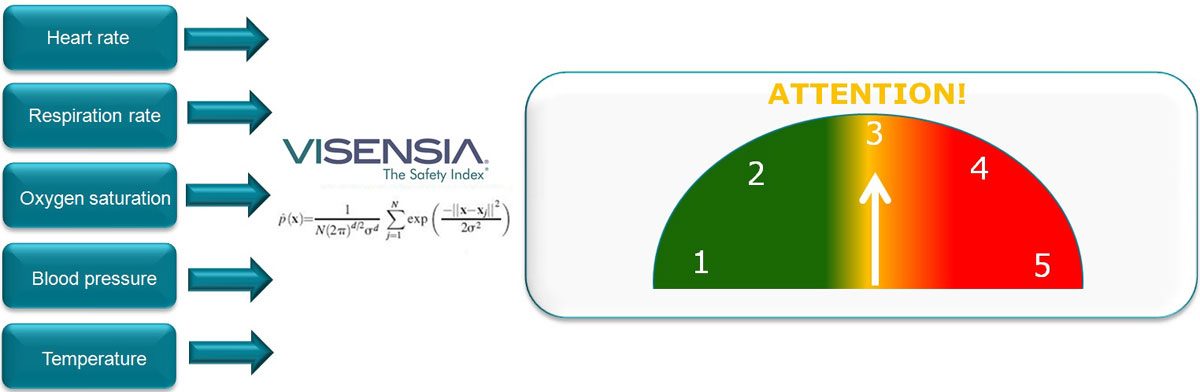
By using modern software, providing 24/7 helpdesk support for users, and linking it to the medical devices (using Artificial Intelligence software systems such as Visensia), we can access the data, analyse the data, and put 24/7 high level nursing care at every bed thereby reducing pressures on nurses and doctors. Using Artificial Intelligence software to monitor the patient and respond early to any signs of deterioration means that, particularly in single room environments such as the Hospital Hotel, lower cost models of care be used to monitor patients with the assurance of 24/7 high quality support.
In summary, healthcare technology is changing current working practices, but the transformation needs to be managed carefully if the systems are to deliver real improvements in productivity.
These new technology solutions can improve NHS best practice and feed into other areas such as producing statistics for reporting and planning future improvements. These technologies will ultimately save time and resources assisting the NHS to deliver better care at a lower cost.
Bibliography
NHS Commissioning Assembly, 2015. Technology Enabled Care Services, s.l.: Quality and Outcomes Working Group - NHS Commissioning Assembly.
NHS Institute for Innovation and Improvement, 2007. Technology to Improve Service, Coventry: NHS Institute for Innovation and Improvement.
NHS Protect, 2015. Guidance for NHS health bodies on the security and management of NHS assets, London: NHS.
Author: Dr John Sandham CEng FIHEEM MIET


