The graph below shows the complex nature of NHS medical equipment inventories in an average 500 bed acute hospital.
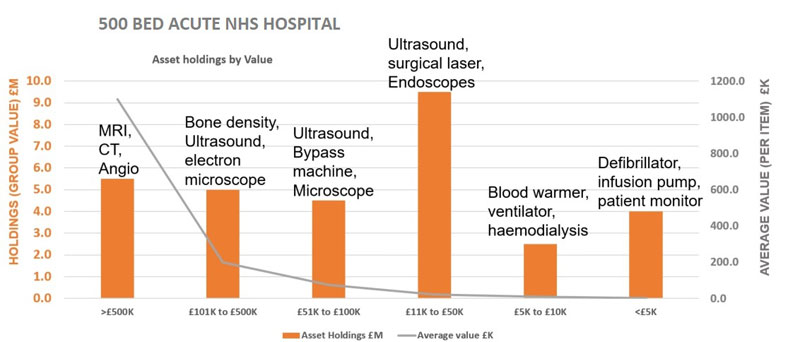
The average healthcare organisation holds a wide variety of devices that may range from low volume / high value items such as Magnetic Resonance Imagers, worth over a million pounds, to high volume / low value items, such as non-invasive blood pressure monitors, worth less than £1000. This graph is a visual example of a UK acute 500 bed Hospital inventory, broken down by Value. The choice of what items to buy is often based on age, rather than having a replacement plan, that is linked to a long-term, operational business strategy. The organisational cost pressures can be offset by investing to save. Investing in the right technology should be linked to a long-term transformation plan, that delivers systematic improvements.
It is common practice in most healthcare organisations to focus on ‘Capital Assets’, this is because they are the most expensive portion of the overall asset holding for a typical acute hospital, representing 85% of the technology spend, but these assets are only 15% of the inventory, by volume. Capital assets are subject to more stringent financial rules than the lower value items under £5000, that represent 85% of the items by volume.

Devices like Defibrillators, infusion pumps, and patient monitors, are usually not considered as a priority for replacement, but they do offer an excellent opportunity to improve organisational efficiency and the future health of the nation. Therefore, any replacement plan should include both capital assets, and asset under £5000 when preparing equipment replacement plans. These plans should go ‘hand-in-glove’ with the strategic goals of the organisation. When buying any medical technology, Health Level 7 (HL7) data transfer capabilities must be considered essential if the ambition of your organisation, is to ensure that device data can be transferred automatically and immediately, into the Electronic Patient Records, thereby improving data integrity.
The complexity that the NHS is facing, and the costs involved, is shown in the graph below.
NHS Asset Holdings

This graph shows that the NHS has 880,500 medical technology assets, with an estimated worth £4.65 Billion. These assets are often kept in operational use long past their manufacturers recommended life. This ultimately reduces spend on technology, but does not improve the efficiency for the organisation, and does not help clinicians to see more patients, or allow them make better clinical decisions.
One question to ask NHS executive’s is: “What if lack of investment stops the organisation moving forward with its long term plans? Executives aspire to use technology to revolutionise clinical care and their organisations efficiency, but getting this right is very challenging.
The UK Health Secretary, Matt Hancock, recently said, “it will be “critical” for the NHS to work with the private sector to continue an uptake in use of technology such as telemedicine, especially after the COVID-19 outbreak has subsided”.
The shift towards digital technology has led to closer working with private sector partners; data-led decision making; and telemedicine projects. The only possible way to bring these new technologies into our healthcare organisations is to have political and financial support for investment in technology. If Matt Hancock is to be believed, the UK has the political buy in and funds will be provided.
Healthcare organisation must also have executive buy in, especially from the Chief Executive, and the board of directors. Matt Hancock recently said when ‘Speaking on The Future of NHS Tech, “We’ve seen the uptake of the use of technology like never before, I’d say the three big areas where there’s been an improvement is telemedicine, data in decision-making, and the teamwork between different institutions”, he went on to Say “We need to entrench these improvements.”
At the moment there are cost pressures on the NHS to save money. With the current asset holdings of £4.65 Bn, the NHS really need to be spending 10% on equipment replacement just to maintain the same levels of technology. Higher levels of investment will be required to deliver the Health Secretary’s ambitions for a technically efficient NHS.
- NHS medical equipment asset holdings = £4.65Bn
- Imaging £2Bn
- Biomedical/Endo £2.65Bn
- NHS annual maintenance spend = £372M
- Imaging £200M (10% of Capex)
- Biomedical/Endo £212M (8% of Capex)
- Estimated NHS annual NHS expenditure on equipment replacement and maintenance
- ((10%*1) +2) = £877M
The current NHS annual spend, just to maintain its current position is a staggering £877Million pounds.
This does not include the further investment required to bring in the more advanced connected systems that are required for the future.
Medical equipment data is a rich source of information that allows better decision making if the doctors and nurses have access to it. It can also guide the senior management on where best to invest their funds to get the greatest benefits in terms of both clinical outcome and financial efficiencies.
The importance of Data
In the NHS, 99% of medical device data generated is not recorded or charted in the EPR (or Trust IT systems where no EPR exists).
It takes between two to twelve hours after collecting vital signs data from patients' monitors before nurses enter it into medical record.
Documentation takes up to 35% of a nurse's time (147 minutes in a 10-hour shift)
Less than 20% of a nurse’s time is spent on patient care and education.
The manual entry of data leads to error rates of 17% (If Clinical decision support software (CDS) is used, it is potentially reporting against erroneous data).
Only 7% of a nurse’s time is spent on patient assessment and surveillance.
6% of patient’s lives are lost in ITU’s because the data we do record is transcribed incorrectly.
We must firstly have accurate data, and the only way to guarantee accuracy is to automate the data entry function. We can then use data to improve services, carry out research, and help clinicians to make better decisions. Improving clinical decision support will ultimately improve the efficiency of the organisation, improve patient care, and reduce mortality.
Part of any medical devices transformational plan must be to connect Medical Devices and medical IT into the Electronic Patient Record (EPR) to ensure clinicians have access to data. This improves the clinical decision making, and ultimately patient care. Connected medical devices push data into the IT systems, reducing errors, and improving clinical workflow. All acute hospitals will eventually have a clinical data centre, that could be likened to an air traffic control centre, with artificial intelligence systems monitoring and managing all the data coming from the patients in the hospital that are connected to medical technology. This centre will have trained clinicians and nurses that can use the Artificial Intelligence to analyse data allowing them to make better decisions about treatment regimes, what drugs to prescribe, and when to discharge.
Some Hospitals are already implementing some of this technology, and these technologies will be in operation in most healthcare organisations within the next 20 years, if the right stakeholder are engaged and a workable funded plan is drawn up, it could happen within 5 years. We need to ensure that any strategic plans include investment in data transfer and AI if improving clinical decision support is part of the plan. The medical director will support this type of investment, especially when it can provide 100% accurate data for doctors, allowing better clinical workflow and smart Early Warning Systems.
One area that has been particularly important during this covid pandemic is remote consultations with patients, thereby avoiding the infection risk of coming to hospital. Remotely operated medical services can be expanded further to allow remote vital signs monitoring of patients, freeing up beds, and avoiding cross infection risks. Telehealth also reduces the number of emergency ambulance calls, because the patient’s vital signs can be seen by both the patient (allowing them to feel reassured) and the doctor (allowing them to make improved and immediate clinical judgements).
In the 1980’s, Asset management involved recording of the individual items within the healthcare organisation, and making sure it was serviceable, the main function being repair and maintenance.
In the last 20 years medical devices have become not only things you can touch, but also software components such as Health Level Seven or HL7, which refers to a set of international standards for transfer of clinical and administrative data between software applications used by various healthcare providers. Hospitals and other healthcare provider organisations typically have many different computer systems used for everything from billing records to patient tracking. All of these systems should communicate with each other (or "interface") when they receive new information, or when they wish to retrieve information, but, at present, not all of them do. HL7 defines a series of electronic messages to support administrative, logistical, financial as well as clinical processes.
 In the next 20 years, data in the electronic patient records or EPR will connect to software systems that use of complex algorithms and software, or in other words, artificial intelligence (AI), to emulate human cognition in the analysis, interpretation, and comprehension of complicated medical and healthcare data. Specifically, AI is the ability of computer algorithms to approximate conclusions without direct human input. The AI conclusions will be immediately available for clinician to review and enhance their own decisions about the clinical care provided to their patients. A typical system will have data being pushed directly from the healthcare technology into the Gateway management software, where it is processed for transmission to the electronic patient record. This is an instantaneous process with 100% accurate data entry. The data can then be used confidently for clinical decision support, clinical research, and finally into AI supported intelligent systems.
In the next 20 years, data in the electronic patient records or EPR will connect to software systems that use of complex algorithms and software, or in other words, artificial intelligence (AI), to emulate human cognition in the analysis, interpretation, and comprehension of complicated medical and healthcare data. Specifically, AI is the ability of computer algorithms to approximate conclusions without direct human input. The AI conclusions will be immediately available for clinician to review and enhance their own decisions about the clinical care provided to their patients. A typical system will have data being pushed directly from the healthcare technology into the Gateway management software, where it is processed for transmission to the electronic patient record. This is an instantaneous process with 100% accurate data entry. The data can then be used confidently for clinical decision support, clinical research, and finally into AI supported intelligent systems.
A small number of UK NHS trusts are already implementing this type of system deployment, but most haven’t yet started. Organisations must understand the benefits of connectivity, only then can they can deliver better patient outcomes, become more efficient, and deliver improved value. The expression “Cost is King” is often used in healthcare organisations, I would disagree, in today’s healthcare world, “Connectivity is King”
John Sandham 2020.


