Thank you very much. So yes, I’ve a background in chemistry, but then worked in the veterinary pharmaceutical industry for about 15 years, so I’m quite new to this world, so be gentle with me. So thank you very much. As a lot of speakers have said already today, it’s great to be actually out in the big wide world and in front of everyone again, though I have to say it might have been slightly more comfortable and less nerve racking being on Zoom hiding behind a screen. So I’m CEO of SageTech Medical. We’re a very young company, been going about five or six years. There are only 12 employees, and I think hopefully today, I mean we’ve seen a lot of diverse talks today already, and I hope this talk I’m about to give will give you some food for thought, and also increase that diverse range that we’ve seen today.
So SageTech Medical as I mentioned was set up five to six years ago, and was set up to address a problem in anaesthesia. So what’s that problem? So that problem is volatile anaesthetic gases. Well actually strictly speaking it’s not a problem with anaesthetic gases; it’s a problem with how we deal with them and what we do with them. At the moment these volatile gases I’m talking about, we’re talking about sevoflurane, isoflurane and desflurane, and these are minimally metabolised. So they’re less then 5% of any of those agents are metabolised. Put it the other way, more than 95% of those gases introduced in the anaesthetic machine are vented through the anaesthetic gas scavenging system out through the chimney of the hospital, so that’s greater than 95% of those are just released uncontrolled into the environment.
So what, you might say. Well let’s just look at the system there. These anaesthetic gases are very damaging for the environment, so if they’re released into the atmosphere they have a big impact. It’s not just that, the current system means that we’re pumping out a lot of valuable anaesthetic gas up the chimney just out into the atmosphere. The model that SageTech is proposing is that these anaesthetic gases are captured before they’re released from the hospital, and they can then in turn actually be recycled. And that could stop over three million tons of CO2 equivalent affecting our environment each year just from that.
So, looking at those numbers a little bit more, as I mentioned the three anaesthetic agents, sevoflurane, desflurane and isoflurane, this table simply shows the global markets for each of those agents, the amount that they’re metabolised or the amount that’s actually released and is wasteful, and then lastly the pollutive impact of those agents in turn. And if we actually hone in on desflurane there, sorry looking at the total, that’s about $1.3bn of value of anaesthetic agents that is pumped out the chimney. That’s pretty wasteful financially in a cash strapped health system, but also if you hone in on desflurane, more than 99% is just pumped out of the chimney. And if we actually then furthermore look at the pollutive effect of desflurane, it’s over five times more pollutive than the other agents. Now, I’m not desflurane bashing here, I’m just saying that there’s a problem with all of them, all these agents. And the NHS is well aware of this. We know that the net zero targets have been published, we know through the very challenging times of the pandemic, that the leadership in the NHS have reaffirmed its commitment to net zero by 2040 for pollution under its control. And it’s been estimated that anaesthesia contributes 5% of that carbon footprint from the NHS, so we can make a real impact by solving this problem.
So how do we solve this problem? SageTech have come up with a solution to try and capture the anaesthetic gas when it’s exhausted or exhaled, and it comes out of the exhaust of the anaesthetic machine. We’ve developed a device, design drawing here, which would attach to the exhaust of the anaesthetic machine, and then the exhaust from our machine would then go into the HSS pendant, thereby venting any excess oxygen, any nitrous oxide that might be being used, and that’s kept away from the operating theatre safely. So we’ve designed this device in collaboration, well we’ve designed the device to make sure it can work together with anaesthetic, major brands’ anaesthetic machines. And what it also has at the top of the device here you can see there’s a small screen there, and what that screen will tell you is how full each canister is that’s loaded into the device. We have canisters, I’ll tell you about in a moment, that capture the anaesthetic, waste anaesthetic gas, and either the screen will tell you each canister in turn, how full it is and when it needs changing. We’ve heard a lot about data today. I don’t want to add to the problem of data that we’ve been hearing about, but that data could be transferred. Whether it’s to the anaesthetic machine, whether it’s to other sources of collecting data, we can send that data from the canisters. Furthermore, if for example a procedure is prolonged in theatre, and you have to change the canisters during the procedure, we are able to hot swap a canister in turn without disrupting the anaesthetic procedure going on.
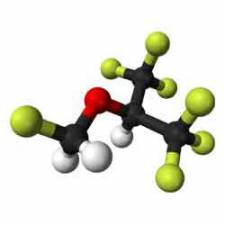
So now just to look at the canisters I’ve mentioned. One of the main tenets of what SageTech has tried to commit on is solving an environmental problem, but not adding to it. But in the solution not generating more further environmental impact. So what we have inside our canisters, which are robust reusable canisters, is a carbon material that is derived from coconut husks, which is a sustainable source. So again this is consistent with our values. The carbon material is very able to capture all three agents I’ve talked about. You can have the canisters in the device, change the anaesthetic gas you’re using during the list in theatre, and our device can capture all three during that procedure. The carbon material is very robust, it can be used many times, in fact we’ve never had a problem with it, we can’t degrade it, but if that were to be degraded we can replace the carbon material inside our reusable canisters, thereby carrying on that sustainability of this solution. And we’ve been able to show capture of anaesthetic gases in various hospitals already around the UK.
So what happens once these canisters are full? We’ve developed another machine, and this we call the extraction machine, it’s not a very fancy name just yet. But it’s about the size of a large wardrobe, and that can be sited close to the theatre suite at a convenient location. It’s fully automated. And it’s also, the canisters are all bar code for asset control, so they can be monitored all the way through the hospital and through this machine. Once the canister is full it can be brought to our extraction machine, loaded in, it’s fully automated and robotic controlled. The canisters then are processed inside the machine and emptied. And when the clinical staff bring a full canister, they take away one that was prepared earlier, because the machine is programmed to be able to run 24/7 as it processes through the canisters. We call them the extraction machine, because the anaesthetic agent is absorbed onto the carbon material very strongly. It’s very stable, so it can be transferred with safety in mind. So what we use to extract off the anaesthetic agent off that material is super critical CO2. And that’s at high temperature and high pressure, where the CO2 operates in a slightly different way, and acts like a solvent to extract off the anaesthetic agent.
Now I want to confirm, again consistent with our values, that CO2 is taken into a super critical state and back down again. And is recycled through our machine, never vented, it’s carried on through, used again and again inside our extraction machine. And as I mentioned we can extract the Isoflurane off each canister, along with the sevoflurane and the desflurane. We don’t want to use single use components in this and consumables, so our model continues to then load the waste anaesthetic we’ve collected off the canisters and load them through to be collected into a large collecting vessel. So everything you’ve seen so far takes place on site in the hospital. Nothing leaves, there’s no carbon footprint from logistics and so on until we get to this point, where we have one single vessel. We estimate for an average hospital every two or so months being transferred to our processing site. So that really minimises the road miles of this solution.
I couldn’t help but show you this slide. The excitement when we were first able to start collecting anaesthetic. This is the anaesthetic being taken off the canisters and being collected in our extraction machine. It did create, as you can imagine after years of development, quite a buzz to see the liquid collecting there. A little bit sad, but it was very exciting for us. Thank you. So the full canister, the full collection vessel then is transferred back to the SageTech site, where we have a mix of isoflurane, sevoflurane and desflurane. We can then filter that, we can separate it and then purify. That pure pharmaceutical can then be rebottled, the necessary MHRA testing, application for a marketing authorisation and then resold as a pure pharmaceutical back into the healthcare system.
By generating that circular economy, we’re able to offer up, potentially offer up savings, we’ve modelled saving to NHS for the cost of their anaesthetic agent. There’s a further knock-on effect here that isn’t obvious. If you start using more and more of the recycled anaesthetic agent, you’re producing less in the first place. And the energy, the manufacturing and any pollution associated with manufacture in the first place is diminished as well, which was an add-on effect of this process. Personally I find it quite incredible, having worked in veterinary pharmaceuticals, it doesn’t matter, the fact that we are talking here about being able to recycle a pharmaceutical is, I can’t think of another pharmaceutical this could happen to, and it’s quite incredible to get your head round I would say.
So, just to summarise part of this, what we believe our solution brings to a number of stakeholders in this anaesthesia process, the hospital, it gives a real win to the hospital. It helps hospitals, the NHS deliver on its net zero targets, and has a real impact on that. The previous talk was talking about visions for the future, and what we can see coming down the line in the future if we can try and imagine. You can start being a lot more flexible in terms of not necessarily having to attach to an AGSS, dependent of course on the oxygen nitrous oxide, but you can start using your hospital space a lot more flexibly, being able to capture the anaesthetic agent. And what I haven’t said already is that we have shown that we capture 100% of the anaesthetic which comes out of the back of the anaesthetic machine. Of course there’s wastage in the anaesthetic room and so on, but everything that comes out of the back of the anaesthetic machine we’ve shown we’re able to capture that. So then you can say operate in time, and we can prove that 100% that we’re able to then move away from the HSS, and be a lot more flexible with design of theatres, and the pop-up theatres and so on.
There’s a knock-on effect of that with cost of electricity, of running AGSS systems, that environmental impact, the cost of installation in the first place, all these things start changing how we think about the setup. Furthermore, I’m not a clinician, but I think there are differences, there are differences in outcomes with different patients with their clinical background or health background on the use of the different agents. Therefore if you start diminishing the cost implications, well certainly the environmental stigma with some of those agents, if you start removing that from the equation, a clinician is able to use the anaesthetic of choice for clinical benefit, which if course has a benefit to them, but most importantly to the patient.
So I’d like to pause for a moment. I started out the talk talking about the problem with anaesthesia, and in fact the problem with how we treat the anaesthetics, there are other problems in anaesthesia, and that’s nitrous oxide. Nitrous oxide is even more polluting than the volatiles I’ve already talked about. Now sadly our technology doesn’t collect the nitrous oxide, but there are technologies available. And whilst we’re not affiliated and connected in any way with the technology I’m about to tell you, I hope you can see why I wanted to mention it, because I think it dovetails nicely, and there’s real synergy between the technology I’ll talk about and what I’ve already spoke about this afternoon.
So there are other technologies that are available. So the technology I’m going to talk to you about just now is from Medclair, which is a Swedish company, relatively small company as well, but they’ve already started selling their solution to solve the nitrous oxide problem. They’ve sold it to over 30 hospitals in Sweden and are looking to start internationalising that solution. So they’ve built up some expertise in being able to measure nitrous oxide importantly, but also being able to crack it, which is using a catalyst to break down the nitrous oxide to its component parts, nitrogen and oxygen, the biggest components of fresh air we breathe. So the output of their machine is essentially virtually fresh air.
So their technology is applicable, as I’ll come on to show, applicable in maternity wards, paediatrics, dentistry. One unit they have is a mobile unit. So, as the name suggests it’s fairly flexible, it can be wheeled around. As you’ll see on this unit it has the cylinders where this nitrous oxide, Entonox, but that can be delivered where pipe gas isn’t available, delivered to the patient as per normal through the mask, and then collected back through the mask into their system that cracks the nitrous oxide as I’ve explained. And that can of course be used in the settings I’ve talked about, in maternity, dentistry and paediatrics. Where the system is slightly more sophisticated, where there’s pipe gas and also it can be collected from a patient in a more traditional way that we might expect with an AGSS and so on, a central destruction unit has been designed, which again is about the size of a large fridge. And that can take input from 16, from patients and 16 maternity rooms, and can take that and crack it in the same way. And these can be stacked up in banks, so it’s very scalable as a solution. Of course there are benefits of this in terms of cleaning up the facility, taking nitrous oxide away from the clinical environment. Again as I’ve said for the volatiles, it can allow, if clinicians want this it can stop the move away from nitrous oxide where there are clinical benefits, where the environment is dictating that move away. They’ve shown they can eliminate 99% of nitrous oxide that goes into their machines, or over that, and it’s very good to have around the system. It’s low noise, low electricity, and very easy to install.
What we’re, well what I’ll finally say is that SageTech isn’t yet selling its technology; we’re going into final trials in a matter of weeks, looking to then C/CA mark our technology, it being ready to then be able to sell our technology later this year, at the end of the calendar year. This is right time as the build-up momentum from the NHS to meet its net zero targets, and as I’ve mentioned already by daisy-chaining our technology and technology like Medclair’s, we can solve a lot of the anaesthetic environmental problems, leading to that 5% reduction in the NHS’ carbon footprint, which just from one small area of the NHS is a significant step.
So, I just want to thank you and John and the organisers for allowing me to come and tell you about SageTech’s mission to take three million tons of CO2 equivalent out of the environment each year from healthcare. Thank you very much for your time.
APPLAUSE
DR JOHN SANDHAM
Do we have any questions?
DELEGATE
Can I just ask you about intravenous anaesthesia, and what the impact for that is likely to be, are people going to go back to the old gas way as they call it?
IAIN MENNEER
Right, so that’s an interesting question. So, as I mentioned a lot of clinicians, I’m not going to sit here and say I sit on one side of the fence or the other. We genuinely have the view that it is then down to clinicians to decide what’s best for what case that they’re dealing with, therefore that’s choice. Bring the choice back into clinicians’ hands. Not having it dictated to as I’ve stressed a bit, because of the environmental problems. What I’d also add is there clearly have been some people that prefer to move to TIVA because of the perceived environmental benefits. Papers are still being published by very eminent scientist anaesthetists that have a particular interest in sustainability, leaders in the US, UK and France that are still stating the environmental impact of propofol is unknown. You can’t capture the metabolites of propofol. There is known to be an impact into the water course of metabolites of propofol. We don’t know what they are yet. I’m saying that openly, we don’t know what they are yet, but it is known. There are high levels of these metabolites being recorded in water courses, and of course there are high levels of plastic waste from TIVA.
So we are very keen. We’ve done work, we’ve sponsored work through an independent university department to look at the full lifecycle analysis of using sevoflurane for example, particularly if you capture it and are able to recycle it. And that’s what we need to get to in this whole discussion, is looking at the full lifecycle analysis of not only volatiles, nitrous, TIVA, to see what the impact is, and where we can minimise that. And then if we’re comparing apples with apples, start getting onto the clinical benefits in that judgement. Long answer sorry, but that’s my take on that.
DR JOHN SANDHAM
I just wanted to say I think it’s incredible to see your technology and what it can do for the environment, and also what it can do for the purse. I don’t think you’ve probably said enough about the cost of anaesthetic agents. Anaesthetic agents are huge, well you said about the global cost, but the impact on an individual hospital could also be substantial. So the cost of anaesthetic agents is huge. I mean the focus is the environment on your presentation, and I really like that. I think we have to consider the environment, and we’re all responsible. We as EBME engineers, technicians, technologists, we appreciate the technology. I liked your video, I thought it was great. And I think that what you’re doing here is probably going to make you a lot of money. That’s good. But also it’s going to save a lot of money for the NHS and it’s going to save a lot of pollution so I’d say well done.
IAIN MENNEER
Thank you.
Iain Menneer's presentation at the EBME Expo: Innovative Technology: Reducing the Environmental and Financial Costs of Anaesthesia