Anaesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical purposes.
Anaesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical purposes.
It may include some or all of analgesia (relief from or prevention of pain), paralysis (muscle relaxation), amnesia (loss of memory), and unconsciousness.
A person under the effects of anaesthetic drugs is referred to as being anaesthetised, and the person giving the drugs is known as an anaesthetist.
What is an Anaesthetist?
Anaesthetists are specialist doctors who are responsible for providing anaesthesia to patients for operations and procedures. In addition anaesthetists have a range of practice which extends beyond anaesthesia for surgery to include pain management and intensive care. Anaesthetists form the largest specialty group of doctors in NHS hospitals. They are doctors who have chosen after qualifying to undertake postgraduate specialist training of at least seven years in anaesthesia, intensive care medicine and pain management.
An anaesthetist cares for you during your operation and will:
- Discuss types of anaesthesia with you and help you to make choices
- Discuss the risks of anaesthesia with you
- Agree a plan with you for your anaesthetic and pain control
- Be responsible for giving you your anaesthetic and for your wellbeing and safety throughout your procedure
- Manage any blood transfusions you may need
- Plan your care, if needed, in the Intensive Care Unit or High Dependency Unit
- Make your experience as calm and pain free as possible
During the 19th century, nitrous oxide, ether, chloroform and ethyl chloride were being used experimentally to alleviate pain experienced during surgery.
The method by which these anaesthetic agents were administered is now considered to be very primitive by modern standards. A major breakthrough was made when apparatus was devised that could control the flow of nitrous oxide and oxygen in adjustable proportions.
Anaesthetic agents that were administered over prolonged periods, in particular chloroform, caused considerable physiological damage to the patients due to their toxicity. A further discovery, trichlorethylene (trilene), made the use of chloroform much less popular. Although much safer it still had one major disadvantage, in that it can not be used in a 'closed circuit' method of anaesthesia. Phosgene, a very toxic gas is produced when trilene flows through the CO2 absorbing chemical soda lime.
Since 1945, a radically different method of anaesthetising patients has become widely practised, based on the discovery that a purified extract of a naturally occurring poison 'curare' can be safely injected intravenously. It produces a muscular relaxation by acting on the patients neuromuscular system.
What does this mean? Various depths of physiological paralysis can be achieved to enable more complex surgery to be carried out. If deep anaesthesia is required utilising this technique, the patients lungs become paralysed and the anaesthetist has to keep the patient alive by controlled artificial ventilation of the lungs.
Modern surgery techniques can sometimes require that a patient is anaesthetised for many hours at the extreme levels of anaesthesia. Previously, this had been a most daunting task for the anaesthetist, and most dangerous to the patients physiologically. The anaesthetist now, has a vast array of sophisticated, reliable, patient and gas monitoring equipment. Closer control in the administration of anaesthetic agents, has now been further enhanced by the widely available compact gas analysers. These can monitor the gases to the patient and also expired gases from the patients lungs.
Anaesthesia
Surgical anaesthesia is a reversible state of unconsciousness produced by drugs, with sufficient depression of the reflexes to allow an operation to be performed.
It can be seen from the above statement that two conditions are necessary before the state of surgical anaesthesia can be achieved. Firstly there should be unconsciousness, which after all, is all that the patient is interested in! Secondly, some depression of muscular reflex activity, which the surgeon needs to enable delicate work.
If an anaesthetic agent is administered in sufficient quantity for long periods, overdose levels are reached which can lead to death. From the time that the first noticeable effect is produced until fatal overdose occurs, the progressive reflex depression of the central nervous system may be divided into four stages.
Stage one
(Analgesia)
During childbirth, some women in labour are administered an analgesic agent (pain relief) and remain conscious and co-operative. Accident victims also need to have some degree of pain relief to lessen the effects of shock. Specifically designed equipment delivers analgesic gas, usually in the proportion 50-50 nitrous oxide and oxygen (entonox).
Stage two
(Unconscious, without reflex depression or delerium)
This is too deep for a woman in labour, as she is required to remain conscious. It is not deep enough for a surgeon as it cannot provide the conditions he requires. This stage is therefore passed through or bypassed altogether.
Stage three
(Unconscious, with reflex depression or surgical anaesthesia)
This provides at its lightest level, sufficient reflex depression to prevent movement of a limb or muscle if the skin is cut.
More anaesthetic agent, and hence more anaesthesia, must be used to depress the more sensitive reflexes, such as those from handling the parietal peritoneum (the abdominal cavity), where inadequate anaesthesia would cause a reflex tightening of the abdominal muscles and prevent the surgeon reaching his objective.
Stage four
(Respiratory paralysis)
Respiration becomes progressively paralysed in the deeper planes of stage three, and when it finally ceases, stage four has been reached. Sometimes the anaesthetist has to take the patients near to the brink of this stage in order to meet the surgeon's requirements.
General Anaesthetic Agents
Nitrous oxide
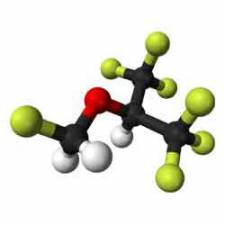
Gas which can be compressed into liquid form. Non explosive, non inflammable. Low toxicity, weak anaesthetic agent. It was used as the sole anaesthetic agent for dental or outpatient procedures. It can be used to maintain anaesthesia during major surgery in combination with other anaesthetic agents; but it is not used on its own to produce a deep level of anaesthesia. Usually administered to the patient in the proportion of two-thirds nitrous oxide to one-third oxygen.
Nitrous oxide mixed in equal proportions with oxygen is used as an analgesic agent for dental surgery or maternity work.
Halothane
Non explosive, non inflammable. Heavy vapour, an organic compound, very potent. Expensive, normally used in closed circuit systems. It is vaporised in special devices that are capable of delivering a calibrated, known concentration. Reduces blood pressure, even at light levels of anaesthesia.
Non anaesthetic gases
Oxygen
Present in the air at a concentration of approximately 21 percent. It cannot be ignited, but its presence will aid combustion. Explosive whilst under pressure and brought into contact with oil or grease. Should not be at administered to patients in concentrations above 40 percent.
Carbon dioxide
It will stimulate respiration making it deeper, but not increasing the rate. Sometimes used when spontaneous respiration does not occur after an operation.
It can also be used, in low proportions to the total gas mixture being administered, as an aid to the smooth induction of anaesthetic agents. (ie. Used with nitrous oxide and oxygen for a short period before using the anaesthetic agent, reduces the patients resistance to breathing in the agent)
Anaesthetic Equipment
 The Boyles apparatus (left) was first developed for use in 1917. It was one of the most common types of anaesthetic equipment used in the operating theatre. It operates on the continuous flow principle whereby gas flows all the time during the inspiratory and expiratory phases of patient respiration, being temporarily stored during expiration in a reservoir bag.
The Boyles apparatus (left) was first developed for use in 1917. It was one of the most common types of anaesthetic equipment used in the operating theatre. It operates on the continuous flow principle whereby gas flows all the time during the inspiratory and expiratory phases of patient respiration, being temporarily stored during expiration in a reservoir bag.
Most gas apparatus in use today is based on the Boyles apparatus, and although dated, the Boyles apparatus is still used in many hospitals.
The basic principles of gas anaesthesia have been known for over a hundred years and are still used. An anaesthetising agent is delivered to the patient via flow controllers and mix controllers. Normally a mix of nitrous oxide and oxygen would act as a carrier for the main agent (i.e. Halothane).
Systemic effects of general anaesthesia
General anaesthesia leads to multi-system physiological changes. The systemic effects of anaesthesia vary with the drugs used so different agents are favoured in different clinical contexts. In general, intravenous (propofol and thiopentone) and volatile agents all reduce blood pressure as a result of vasodilation, and negative inotropy and chronotropy. Starting positive pressure ventilation (i.e. ventilating someone) can impede venous return to the heart, reducing preload and cardiac output. The sympathetic stimulation from surgery opposes these changes.
Intravenous (propofol, thiopentone and etomidate) and volatile agents are all respiratory depressants and depress airway reflexes to differing degrees. Propofol is particularly effective at inducing transient apnoea and depressing airway reflexes facilitating placement of supraglottic devices post induction. Of the volatile agents, sevoflurane is the least irritant to airways making it particularly suitable for gaseous induction and paediatrics. Desflurane is irritant and is therefore often used once anaesthesia and airway have been established. Both sevoflurane and isoflurane are bronchodilators and may even have a role in the management of brittle asthma. Ketamine is an exceptional intravenous agent in that it maintains cardiovascular stability and preserves muscular tone, airway patency and bronchodilates in addition to its analgesic properties. It is termed a ‘dissociative anaesthetic’, meaning the patient may be unaware and detached from his/her surroundings but not completely unconscious. Its attributes make it useful in haemodynamically unstable patients, the developing world and field anaesthesia.
Emergence and recovery
Once anaesthesia is no longer required, maintenance agents can be switched off. Before emergence, adequate analgesia and anti-emesis should be ensured and neuromuscular junction function restored if a muscle relaxant has been used. Like induction, emergence can be a time of physiological disturbance. As patients start to wake from anaesthesia or ‘lighten’ they may develop agitation, laryngospasm and breath-holding.
Conventionally extubation is performed following oropharyngeal suction, once the patient is generating good tidal volumes and is awake, ensuring airway reflexes have returned and the patient will protect his/her own airway. In certain circumstances extubation may be performed ‘deep’, i.e. with the patient still under anaesthesia. Under anaesthesia, airway reflexes will remain suppressed, reducing the risk of coughing, laryngospasm and hypertension associated with extubation. This may be preferable in certain neurosurgical and cardiac patients in whom surges in intracranial or systemic blood pressure should be avoided. However, the airway will be unprotected against aspiration until the patient is awake.
The recovery room is an intermediate place of safety between theatre and the ward where immediate surgical or anaesthetic complications can be detected and managed. Vital signs, pain scores and other potential problems such as postoperative nausea and vomiting are monitored.
https://en.wikipedia.org/wiki/Anesthesia
https://www.draeger.com/Products/Media/draeger-perseus-a500-anaesthesia-machines-3-2-D-90970-2013.jpg
https://www.ucl.ac.uk/anaesthesia/sites/anaesthesia/files/IntroductionToAnaesthesia.pdf