Good morning, my name’s Joe Emmerson. I’m the Technical Manager for Manchester Foundation Trust. I’m glad that I’m first on. There’s probably an 80% chance that you’ll all be awake by the end of the presentation, so that’s wonderful. Having spent 13 years in the MOD and followed up by 16 years in the NHS thus far, as medical and dental technician, as an EBME engineer or an electronics engineer, I think I’m well-equipped and well-presented really to be able to talk today about Manchester Foundation Trust. I thought it would be quite good preparation really, quite a considerable amount of years before joining the trust to equip me for what is quite a colossus organisation. It’s absolutely huge. And as we go through the presentation I’ll try and explain what Manchester Foundation Trust looks like, how big it is and how it came into being as an organisation, and obviously the challenges which that imposes on myself in order to manage it. I’m not here to promote a product. I’m not here to sell anything or introduce any new exciting technology or anything like that; I’m just here to explain what it’s like managing a trust of that size and the sort of difficulties I’ve had, particularly over the last two years and particularly the last 18 months in particular.
So a lot of what defines a trust is about the structure and the culture. And I’ll cover that quite a lot in the presentation, because I think it’s important to remember that Manchester Foundation Trust is a new organisation as such. It’s constantly evolved to where it is today, and I’ve had to take that into account when managing the transition and the change management throughout the organisation. So I’m going to run through my organisation from 2009 to present. I’ll do it fairly briefly, but it gives you a feel as to how the component parts have been put together. I’ll talk about the challenges, how we’ve addressed the strategy through that and what progress I’ve made to date. This is an 18 month journey. This isn’t an 18 year journey for me; this is a fairly short journey.
So Oxford Road campus - in 2009 what was Central Manchester Foundation Trust commissioned one of the largest PFI schemes in the NHS, bringing together a campus of sites of five hospitals. There’s Manchester Royal Infirmary, everybody seems to know Manchester Royal Infirmary, but what some people often forget is that there’s four other hospitals connected to that campus. There’s Manchester Royal Children’s, a 371-bed hospital, and it’s the largest freestanding children’s hospital in the UK; St Mary’s Hospital, which concentrates on women and neonates; Manchester Royal Eye Hospital; University Dental Hospital of Manchester. At the time the EBME department at Oxford Road campus used a locally developed system for their medical device management, which was a Microsoft Access based system that included inventory, orders, asset management, time logging, annual leave, etc. And that was in use from around about 2000 all the way through to 2016. So there’s quite a significant culture built into the department of a very bespoke product. And anyone who’s been at Central Manchester will probably have seen that system. Oxford Road joined Trafford General Hospital in moving across to the EMAT system in 2016. So again that’s still fairly new in the last five years.
When we look at Trafford General Hospital and Altrincham, which is one of the children’s sites of Trafford General Hospital, Trafford General Hospital joined Manchester Foundation Trust in 2012. Altrincham always came under the care of Trafford, and it was rebuilt on a new site in April 2015. You could say it all started here. For those that don’t know on the 5th July 1948, Trafford General Hospital became the first hospital in the UK, in the world in fact to offer free healthcare, and that was known as the birth of the NHS. On 5th July 1948 Mr Nye Bevan opened, and he symbolically received the keys from the county council to open the site as the first NHS site, and the NHS has continually evolved and continually changed ever since that date. You’re already sensing quite a strong culture from Trafford General Hospital from Oxford Road campus, the site, and in fact even the individual sites within the organisation on that particular campus.
Taking that a little bit further, University Hospitals of South Manchester Trust, UHSM joined Oxford Road campus and formed Manchester Foundation Trust for the first time on 1st October 2017. UHSM in itself is a significantly sized organisation. It’s a major acute teaching hospital providing services to the adults and children throughout Wythenshawe and Withington Community Hospital. Wythenshawe Hospital had got specialist focus in cardiac services, heart and lung transplants, and respiratory medicine. Interestingly the EBME department themselves actually didn’t come across to me until July 2019, almost within my first month of joining Manchester Foundation Trust. The first task was to tupe 22 staff, 5,000 employees in an 800-bedded hospital into Manchester Foundation Trust. USHM were the last recorded user - I’ve been informed very well about this - the last recorded users of the Philips Optim database until switchover to a new supplier in January 2020.
Then we look to the community. Now most organisations have one community attached to them. And in fact Manchester Foundation Trust now have 10 hospitals and two communities attached to them. Manchester Local Care Organisation was the first one that was formed in April 2018 as a partnership between Manchester Foundation Trust, Greater Manchester Mental Health, Manchester City Council, Manchester Health and Care Commissioning, and the Manchester Primary Care Partnership. Trafford Local Care Organisation was formed on 1st October 2019, and it provides a community health and acute and social care for the neighbouring borough of Trafford. You can see within the Manchester region all these organisations coming together in quite a short amount of time, all on different systems, all functioning completely differently, and we’re going to try and make this work as an organisation as a single entity.
As if things weren’t busy enough, on 1st April 2021 the North Manchester General Hospital split away from Pennine Acute and merged and joined, or was assimilated into Manchester Foundation Trust - the final aspect of delivering a single hospital service across the whole of Manchester and Trafford. Again North Manchester is a fairly reasonably sized site. It’s a 500-bed, inpatient beds, approximately 3,300 staff, and 13 staff came across to join my EBME department. There’s been a significant amount of work, despite all the pandemic and everything else, to incorporate North Manchester General Hospital into our structure, to go through the due diligence, and a significant amount of work to restructure and make sure things are put in place to be able to support the organisation from day one, and currently they use the EMAT database.
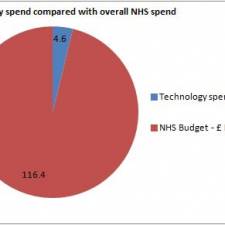
All these organisations now, and all these sites, departments, 10 acute sites and two community settings, all the different systems, the different staff, have come together to form what is now known as Manchester Foundation Trust. It is the largest trust in the UK. There’s 10 hospital, two community organisations, 25,000 staff, approximately 25,000 staff, and approximately a budget of £2 billion. In the previous slide you’ve seen in the last three years there’s been significant amalgamation, significant consolidation as part of the move towards a single hospital service. And that’s a scary thing. In the last three years the organisation has doubled in size with the assimilation of UHSM, Wythenshawe Hospital and North Manchester. Hospitals in themselves, unusually within our organisation have their own chief execs, their own governance structures, their own directors of finance within each individual hospital. In addition to this overarching across the whole group of hospitals is a group structure in a similar manner. So you can see how complex it will be to try and get things done in an organisation this colossus. Having Googled and to put things into perspective, if these figures are correct that is, Sheffield Teaching Hospital is probably the second largest in the UK, with five hospitals, 16,000 staff and a budget of approximately £1.2 million, so in contrast this is massive. Had the organisation told me how big it was before I joined, I may have thought differently about joining them etc., but it’s been a really exciting journey, certainly for the last 18 months.
The next slide is probably too difficult to see because of the amount of stuff on there. What I’ve attempted to do is portray what my organisational looks like in terms of the EBME department. We have four separate entities, which is Wythenshawe Hospital, Oxford Road campus, Trafford General Hospital and North Manchester as three individual EBME departments. Obviously Oxford Road is the largest. It contains five sites in the one campus. Overarching across those structures is a new structure; whereas before there wasn’t an overarching structure across all the sites. This is something that I’ve had to put in place to try and make it work across the organisation. We did have or currently have three database systems. Two systems have transferred across to the EQUIP system. Wythenshawe went live in January/February 2020, again in the last 18 months. Oxford Road and Trafford went across in April 2020. That’s three months apart. And for those that have been involved in database transfer and new systems that’s some going. North Manchester came onboard in April 2021, only a few months ago. We’re hoping to go live with them maybe September. We’ve now got 80 staff working in the EBME department. We’ve got a budget of approximately £6 million, and we’ve got between 70-80,000 pieces of medical equipment across the trust that we have on our inventory. There’s probably a few more on contracts etc., but that’s what we’ve got on our system.
So what does that look like in terms of challenges to such a massive organisation with the significant inherent challenges and difficulties of assimilating this into a functional entity? Well for starters when I joined the organisation on a secondment 24 months ago I inherited what was the CQC action plan. And if you’ve ever been involved in a CQC action plan following a CQC report, there’s a lot of work involved. Unfortunately for me I joined at a time when it was an action plan already in progress, and it was a 12-month action plan, and I joined at the six month point with 12 months’ worth of work to do. The push was to harmonise the medical devices policies, as there were multiple policies across the organisation. There were multiple databases across the organisation, and there were multiple ways of working across the organisation. And so the CQC recognised this and quite rightly said you need to do something about it, you can’t just keep bringing new sites in, and expect the policies not to be harmonised and synchronised etc.
In the last, in terms of cultures, I think this is really important. Every single site has got its own unique identity. It’s got its own inherent way of doing things and of course every site is right. There’s a lot of emotional attachment to the way that things are done. There’s a lot of baggage, there’s a lot of loyalty. And just as an example to this, I attend three medical device management meetings, three medical devices groups. We have a group medical device management committee, which I chair. We have a medical device management group within the community, and we have a medical device group within the Manchester Royal Infirmary. I’m just hoping all the other sites don’t follow suit and set up their own medical device management groups and expect me to attend them. There’s that pressure. I’m all for managing medical devices, but I choose not to chair for all the hospitals, it would be impossible.
In terms of acquisition and expansion, the changes to the development, I talked about Wythenshawe and North Manchester having merged into Manchester Foundation Trust. My team has doubled its size in the last 18 months. And it’s taken considerable time, effort and dedication, despite all that’s been going on in the last 18 months, to get that over the line. If you’ve been involved in any acquisitions and mergers, the amount of due diligence involved etc., it’s really difficult. In terms of the infrastructure, again this is a significant challenge. We’ve got Oxford Road and Wythenshawe, who were both running old database systems when I joined the organisation. North Manchester adds yet another aspect to that. Imagine files and folders and 20 years’ worth of information from each organisation collated in different locations, and actually just being able to access those from the different sites was in some cases physically impossible, because of the network infrastructure.
Structurally, there wasn’t a cross-site team. There were silos. There was Oxford Road, Trafford, Wythenshawe, North Manchester - that’s been a challenge in itself. Moving on to capital, which is probably the bane of most people’s life, because of the complexity of the organisation, and each site having their own views and their standpoints on equipment standardisation, strong views that is, strong clinical views, and even between the sites complete opposition, coupled with our weak links with procurement meant that the involvement of medical device management team or the medical device and medical engineering teams in decision making was fairly poor.
Think about the variance of technical training. We’ve got somewhere in the region of 5,000 different models of equipment throughout the organisation on the three, in fact I’ve not looked at North Manchester’s data, there’s probably more, 5,000 models of equipment. It’s practically impossible to get staff trained on every single piece of equipment. And we had a poor mix of generalism versus specialist engineers. Everybody wants to be a specialist engineering, nobody wants to work on a wide variety of medical equipment, and so there’s challenges around the workforce and the development of that.
Within the sites themselves, the working relationships just on the sites, looking at the management of staff, the relationships between staff themselves, and the relationships between the sites, even within the EBME department, there was a difference of opinion, a difference of cultures, a difference of ways of doing things. And some people said it’s difficult to herd, herding consultants and getting consultants to agree on things on difficult, it’s like herding cats. Try doing that within an EBME department spanning across five different sites with 20 years’ culture and heritage attached to that. That’s difficult in itself.
I was the new guy coming in on a secondment 24 months ago. And when you’ve been in an organisation for a long time, you understand it’s easy how to get things done. You know which people to pull, which favours to call in, where all the holes, the nooks and crannies, and where all the problems are, the inherent problems. There’s been a history of MFT revitalising itself. There’s been heavy HR involvement, you know, engagement sessions and so on and so forth, but the pattern, they’ve never really quite got it right, and just adding those sites hasn’t fixed it any more. So yeah it’s been difficult. A very tough crowd, a very difficult bunch to deal with, with very strong opposing opinions, even between the sites, never mind my opinion versus their opinion, and I always feel that going back to the army days, the general of an army is only as strong as the people who are willing to follow them. So for me it’s been very challenging, very hard mentally and physically, especially given the distances involved when I was commuting to Manchester on a daily basis, it was a two-hour commute in, a two-hour commute back. That’s a five o’clock start and an eight o’clock finish. This is live, eat and sleep Manchester Foundation Trust.
So, let’s look at the big things that we’ve actually achieved in the last 18 months, despite the organisation, despite the way that it’s been formed and despite the cultures. The database go live, six months, six months in to joining Manchester Foundation Trust we went live with, in addition to the CQC action plan, we went live with EQUIP at Wythenshawe in January 2020. Three months later in April 2020 we went live with our second installation across Wythenshawe; both sites having approximately 30,000 devices each and that’s a significant move. And most people would say well that’s not too bad, you know, why didn’t you go onto the one system? When you think about the rationalisation between the two databases, everyone calls a different device something different, the systems have been set up completely different, different job types, different companies, different processes. We’ve moved over to two systems. That took a massive amount of data cleansing, a massive amount of work.
Next is the Nightingale Hospital. Around the time of the go live of the EQUIP system, if you look at the second installation, which is April 2020, nine months in of the Oxford Road campus, Nightingale North West appeared almost overnight. Well two weeks in fact to form a 500 bedded hospital. Thankfully the original involvement from MFT as the host organisation was fairly limited, because specialist companies, thankfully to Caroline Finlay from MTS - useful plug there. They came in and they rapidly commissioned the entire site, rapidly procuring lots and lots of medical equipment over a short period of time. I was heavily in that, but only at a strategic level, so I didn’t need to operationally get involved. I was more involved with the procurement side, and forging the links between the host organisation and the rapid commissioning team. However that got handed over to us fairly soon in May, and we had to very quickly pull on agency engineers, put structures in place, and I’ve got to thank those involved. I had some really good staff who got stuck into the Nightingale Hospital and took over a lot of the leadership aspects of it, because operationally it was a challenge to set up a new EBME function at the drop of a hat. As we transferred from rapid commissioning to operational that posed something new to us. We’d never done it before. There was no lessons to learn from anybody else, we had to do as best as we could in as short a time as possible.
Almost adding insult to injury we had COVID, everybody’s had COVID, this is has affected all NHS trusts. But in an organisation the size of mine this hits us multiple times and in multiple ways. For many reasons staff attendance was poor, prolonged absences, vacancies of skilled staff was fairly prominent. We’ve just taken on Nightingale North West. We’re trying to push all the new database systems, new ways of working, and our staff are dropping in numbers significantly. Procurement added to that problem, all the capital funding, and I’m sure many organisations happened, all the capital funding from 2020 miraculously became available, and then what also happened is all the funding from the next year, 2021, got brought forward, and so we had a massive influx of equipment from the capital programme.
Our goods in area was full on a daily basis, and we were struggling to manage the rapid acceptance testing. And we actually drew a halt to planned maintenance for a period of time, just to be able to cope with those workloads. Depleting staff, masses and masses and masses of equipment in pallet loads, truck loads. And further NHS England pre-emptively sent equipment to lots of major acute hospitals, like it or not NHS provided it to us, and we were already struggling for space. And trying to track orders, commissioning and bring things in in a safe way during that time has been incredibly challenging for us all. We’ve had to form really strong links with procurement, and in some cases both us and procurement have been scratching our heads when somebody else decides to send some equipment into the organisation.
It would be remiss of me not to mention the MPSA alerts that have affected us this year. It’s been a difficult year. It’s been a difficult time. We’ve had some MPSA alerts over the last three or four months. A few months ago some of the knock-on effects from the MPSA alerts accelerated what was already an ongoing replacement programme for infusion devices. I’m sure many trusts have been affected by it and made different plans etc., but the programme of evaluation, training and rollout meant that we brought in just under 4,000 infusion pumps into our trust in a very short time, and that’s working closely in partnership with the companies that are providing the devices to make sure that it’s done in a safe and sensible way. This involved leadership at significant senior level, cooperation between ourselves, procurement, finance and the clinical users.
And who’s had to coordinate that? Mostly the medical engineering department, because we’re the ones that have got the information, we’re the ones that have got the links with the suppliers. Finance want to buy the stuff, procurement want to get it delivered to us, the end users are too busy, so we ended up controlling and managing that rollout. Just looking at the impact of a more recent MPSA alert, and due to the size of the organisation that we’re in, we also need to get involved in that and plan that. Again things keep coming in, the new day job is to deal with the emergencies that present themselves, and I think we’re getting quite tech savvy having to pull that information across the three database systems that we currently run.
Just getting through the last 18 months has been an achievement in itself. I’m sure many NHS trusts and EBME organisations and departments feel exactly the same way. You all deserve an applaud and a well done. It’s been a significant journey. We’ve completed within MFT the work on the CQC action plan. We’ve restructured the department across the sites. We’ve had many internal promotions and lots of movements, vacancies, and there’s lots of recruitment still ongoing to fill what is now going to be the MFT structure moving forward. We’ve gone live with two instances of database systems. We’ve shared and rationalised information between those two systems to work cooperatively together, and try and add some interoperability between the sites. We’ve acquired North Manchester, we’ve acquired Wythenshawe, and we’ve rotated some of our senior management team between the different sites to start to try and understand relationships between the sites and improve working relationships in general.
We’ve improved significantly our relationships, which is absolutely key with procurement, and we’ve now got I would hope a very strong involvement in purchasing decisions. And if there’s any suppliers here today listening to the presentation, I would say if you want to supply equipment to Manchester Foundation Trust, then make sure technical training is included, because we’ve pushed this back to the suppliers many times. Because what tends to happen is the equipment floods in and then we pick up the pieces afterwards, so we’ve included that as part of the procurement exercise for all suppliers.
We are and have been doing, invested a significant amount in safe training. Over the last 12 months not many suppliers were able to provide technical training for our staff, because of COVID etc. etc. We’ve now got quite a significant backlog of technical training. We’ve purchased somewhere in the region of 15,000 devices over the last year, year and a half, and we’ve invested heavily in booking training courses for all those staff to rapidly upskill them and give them a greater breadth of experience. Our priorities and our strategy haven’t just been made up, we’ve planned this fairly well, and that’s been to focus on bringing the database systems together, or at least bring them onto the same platform, on the same server, looking at our file storage in locations. And an example of that, it took me five months to get our IT department to set up an appropriate structure with appropriate links and permissions and access rights to a folder that medical engineering could share, because of the complexities of the organisation, five months - and making working processes and access to information as easy as possible. Now that all sounds very interesting and very challenging, and I want to show you some of the things that MFT have done, how we’ve actually applied some of this, it sounds very good in theory, but I’d like to demonstrate some pictures and say what we’ve actually done in order to make that happen over the last 18 months.
In addition to surviving the last 18 months, fixing all that life had to throw at us and developing ourselves round the big challenges, which I’ve previously discussed, we also took the time to begin the difficult job of bringing the sites together, and share some of the common ground and some of the common practices. Chris Gale talked yesterday about human factors, and I believe in human factors as something which is really beneficial. And what you see before you is a piece of software, let’s call it a launch pad, or if you make it available, you make it obvious and you make it completely unavoidable, and staff are unable to hide from it, then there’s a good opportunity, there’s a good chance that staff may actually use it.
What we’ve developed is a launch pad application. It’s just a digital pathway to every piece of software that we may use, all the links to the folders etc. It ensures that staff are mapped to the same drive letters and locations, regardless of where they log on to, and I’m sure many of you have logged into active directory, and you’ve struggled to find what’s the G drive or the M drive or the H drive. This application will automatically map your drives, will connect you to the database and will give you a shortcut to all the applications, depending on which site you’re working on. You’ll see at the top there Oxford Road, Wythenshawe, Trafford, each site has got its own list of frequently used applications. This has been developed in-house by myself and by some members of the team and support.
In addition to being a launch pad for various bits of software, the majority of these pieces of software are bespoke. We’ve also created applications to undertake fairly common tasks. So for example we can see we’ve got a shortcut to our EQUIP database in the top left there. And as we switch to Trafford General Hospital or the Wythenshawe General Hospital, if you click on EQUIP it will take you to the EQUIP of that particular site, so there’s no need to switch between databases and things like that.
We’ve got Report View application, which is a categorised library of premade reports, which is accessible to those with less confidence in IT. We’ve got an Address Book application, which I’ll cover. We’ve got a drop panel, which gives us the ability to attach documents to jobs, models, contracts, etc. We’ve got a calculator for devices of residual value, which automatically pulls lifespan and data, purchasing data from the database systems. We’ve got a structure. We’ve got email groups. What’s interesting, you can see a little icon there for device de-commissioner. Now we probably scrap in the region of 7,000 devices a year. That’s our churn, 7,000 a year. Now if we can shave a couple of moments of time off that by rapidly decommissioning or rapidly acceptance testing, then it’s useful to have an application to do that. And some of the other tabs I’ll cover in just a second.
It looks very simple, but one of the most difficult challenges was actually remembering who’s in the organisation, who’s in the EBME team, with 80 staff it’s constantly changing. So we developed a very small app to enable us to be able to email various groups of staff. Admin, management, all staff, contractors, etc., across the various sites, and that’s been absolutely fabulous. We’ve developed an address book which combines company contact details, individual contact details and site contact details all into one system. But actually not just that, it’s actually integrated into our EQUIP database. It connects, reads and writes from the system, but I think it presents it in a better way, a more useable way for us to be able to manage our suppliers and contact details. Later on down the line we’ll be using that to automate a lot of the messages from and to the systems. And staff are now less inclined to keep their own list, their own contact list, everyone’s got their post-it notes.
We’ve also introduced a service manual archive, where we will hold a single resource for service manuals, PVPs, check sheets, device configurations, passwords. It’s database agnostic. You can have result sheets in there, returns forms for equipment etc. Duplications minimised, and all sites are able to feed into this as a single resource from a single access point, which makes it really useful. It’s presented in a way you can visually see the equipment, and there’s going to be a lot of work integrating all the different sites’ service manuals, archives into the single place. More recently we’ve developed an online reporting system. We persuaded our IT department to give us our own reporting server, and we can upload specific live reports to enable our customers to be able to obtain the inventory listings to do, housekeepers to use validation checks. We’re just about to upload a device tracker and a model finder so that if you find a piece of equipment and type in an asset number, you’ll get the full history of it and find out who it belongs to.
These are fairly simple things, but in an organisation the size of Manchester Foundation Trust, with an IT department as dysfunctional as it is, these have been quite significant challenges. Built into this system again is just a dashboard panel. We’ve got My Jobs, which displays for each engineers the one stop shop for which jobs are open, how long they’ve been open, when did I last spin the plate or make a phone call about that piece of equipment, what did I do? And it allows a structured discussion between the manager and the individual about their workload. When we first set this up and looked at the data, it was awful, absolutely awful. So we’ve gone through many data cleanses, many old jobs on the system to clear this through. You can imagine 20 years’ worth of inherited data to work through.
So this is presented to them on a tab. And the last one there is a little bit of instant feedback about an individual’s performance. There’s a tab there which gives for our engineers, it tells them how many jobs they’ve got open, their productivity, the quality of their work. It’s a live data checking tool to look for any jobs, various conditions, and it gives the instant feedback to them, because we want staff to be able to manage themselves and be more agnostic from their managers so that when we’re having a conversation with staff about their performance, it shouldn’t be a surprise. And it provides a yardstick of measure for all staff in exactly the same way.
So I hope this gives you the insight in what it’s like developing and managing a large NHS EBME department, it’s been a significant challenge to me in the last 18 months, and I hope you can see what kind of progress we’ve made within MFT, despite all the challenges. Despite the pandemic, despite everything else that the world has had to chuck at us, we’ve made quite a lot of progress in the last 18 months.
Thank you.
Joe Emmerson's presentation at the EBME Expo: Developing a Large NHS Clinical Engineering Department