The impact of the CQC and NHS Resolution on medical devices management.
What do healthcare organisations need to do with their medical equipment management policy to meet the regulations and standards?
 Diagnostic and therapeutic equipment is used every day by most healthcare professionals in the course of their work to support the treatment and care of patients.
Diagnostic and therapeutic equipment is used every day by most healthcare professionals in the course of their work to support the treatment and care of patients.
It is the responsibility of each organisation to ensure that healthcare professionals are using equipment safely and for the purpose it was intended.
The delivery of safe and effective treatment in healthcare settings is dependent on the correct use of medical equipment in a range of applications.
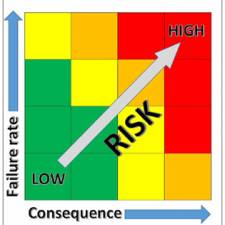
These interventions can optimise treatment, reduce length of stay and improve the patient experience of care. However, when used inappropriately medical equipment carry the associated risk of causing harm to patients that can, if unchecked be serious.
It is therefore essential that all organisations have an overarching medical equipment policy and training programmes to minimise the risk of errors occurring.
Healthcare Organisations are constantly under pressure to improve processes and enshrine those processes within their organisational policies. The importance of policies to the individual, the Department, and the organisation cannot be understated.
The core bodies that healthcare organisations in the United Kingdom are most concerned with are:
- The Care Quality Commission (CQC)
- Medicines and Healthcare products Regulatory Agency (MHRA)
- NHS Resolution (NHSR)
- The Care Quality Commission audits against health and social care act regulations approved by the United Kingdom government. A summary of the regulations that impact on medical equipment management policy is described later in this document.
- The ‘Managing medical devices (2014)’ document is an excellent guide to creating good policy, and enabling best practice. It outlines a systematic approach to the acquisition, deployment, maintenance (preventive maintenance and performance assurance), repair and disposal of medical devices. It is intended for people in hospitals and community-based organisations that are responsible for the management of reusable medical devices.
- NHS Resolution (previously called the NHS Litigation Authority) sets out how the NHS will build upon its strengths to transform the way in which NHS resources will benefit patients, resolve concerns and help to improve safety.
NHS Resolution sets the risk management standards for the Clinical Negligence Scheme for Trusts (CNST). The objective of these standards is to make the patient environment safer. If organisations are members of the NHS Resolution scheme (all NHS organisations must be members) the goal must be to reduce risk by providing evidence to the auditors that they are complying with the standards.
Both the NHS Resolution and the CQC base much of their audit criteria on information provided by The Medicines and Healthcare Products Regulatory Agency (MHRA)
Many Organisations struggle with changes in regulatory standards. Some organisations do not have systems in place that enable them to quickly change and implement policy. Therefore changes made by government may never actually get down to organisational level policy, in a reasonable timeframe.
If an organisation does not have professionally qualified clinical engineers that are able to interpret the changes in regulatory standards and then update the organisational policy, the changes required by government will not be implemented. Even if the organisation does have professionally qualified people able to interpret the changes in the standards and update their policies, this in itself does not mean the policy will be implemented.
Many organisations have policies that are not fully implemented. The managers responsible for understanding and implementing policy need a support structure that can communicate any changes and assist them to implement those changes.
The interesting question might be “How do we make medical equipment policy work?”
I have carried out hundreds of audits on medical equipment policy. Many of the individuals expected to practice in accordance with the policy have not read the policy document. The practitioners expected to work in accordance with the policy have often received no training on the requirements of the policy. How can we expect them to implement the policy without the knowledge of what it states?
In my experience, many organisations expect the practitioners to work in accordance with the ratified policy without any meaningful involvement in developing policy. The often therefore feel disassociated from the policy. As experts in medical equipment management what should we be doing to improve the situation?
In my experience, going out and speaking to the stakeholders who actually buy, use, or maintain equipment can result in a policy which is a useful ‘living’ document (as opposed to sitting on a shelf gathering dust). If the stakeholders actually understand policy, it makes it easier to implement, and more successful in reducing risk and creating a more efficient organisation.
There are three steps to improving compliance with regulatory standards for medical equipment policy:
1. Ensure the organisation has a medical equipment committee which is representational of all professional groups involved in buying, using, maintaining, or managing medical equipment. This group should ensure policy compliance.
2. All Ward and departmental managers should receive training on the policy to ensure they understand their responsibilities and are able to cascade their knowledge and skills to their teams. A professionally qualified medical equipment manager should be responsible for delivering that training, and supporting the managers to implement at a Ward and departmental level.
3. The organisation should ensure that the policy is monitored through a focus group to ensure wards and departments have understood the policy, and are able to feedback to the medical equipment committee any issues with regards to implementing the policy, or any ideas for improving the policy.

Medical device
The term ‘medical device’ encompasses medical devices as legally defined in the Medical Devices Regulations. This refers to an instrument, apparatus, appliance, material or other article, whether used alone or in combination, together with any software necessary for its proper application, which is intended by the manufacturer to be used for the purposes of:
− Diagnosis, prevention, monitoring, treatment or alleviation of disease;
− Diagnosis, monitoring, treatment, alleviation of, or compensation for, an injury or physical impairment;
− Investigation, replacement, or modification of the anatomy or of a physiological process; or
− Control of conception.
A medical device does not achieve its principal intended action in or on the human body by pharmacological, immunological or metabolic means. This definition includes devices intended to administer a medicinal product, such as a syringe driver, or which incorporate a substance defined as a medicinal product, such as a drug-eluting stent.
The relevant CQC outcomes for medical equipment are:
Outcome 8 - Cleanliness and infection control (Core standard 12)
(1) The registered person must, so far as reasonably practicable, ensure that— (a) service users; (b) persons employed for the purpose of the carrying on of the regulated activity; and (c) others who may be at risk of exposure to a health care associated infection arising from the carrying on of the regulated activity, are protected against identifiable risks of acquiring such an infection by the means specified in paragraph (2).
(2) The means referred to in paragraph (1) are (a) the effective operation of systems designed to assess the risk of and to prevent, detect and control the spread of a healthcare associated infection; (b) where applicable, the provision of appropriate treatment for those who are affected by a healthcare associated infection; and (c) the maintenance of appropriate standards of cleanliness and hygiene in relation to:
(i) premises occupied for the purpose of carrying on the regulated activity,
(ii) equipment and reusable medical devices used for the purpose of carrying on the regulated activity, and
(iii) materials to be used in the treatment of service users where such materials are at risk of being contaminated with a health care associated infection. Regulation 12 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2010
Outcome 11 - Safety, availability and suitability of equipment (Core standard 16)
(1) The registered person must make suitable arrangements to protect service users and
others who may be at risk from the use of unsafe equipment by ensuring that equipment
provided for the purposes of the carrying on of a regulated activity is—
(a) properly maintained and suitable for its purpose; and
(b) used correctly.
(2) The registered person must ensure that equipment is available in sufficient quantities in order
to ensure the safety of service users and meet their assessed needs.
(3) Where equipment is provided to support service users in their day to day living, the registered
person must ensure that, as far as reasonably practicable, such equipment promotes the
independence and comfort of service users.
(4) For the purposes of this regulation—
(a) “equipment” includes a medical device; and
(b) “medical device” has the same meaning as in the Medical Devices Regulations 2002.
What standards are NHS Resolution focussing on?
The risk standards impacting on medical devices management are:
• Standard 5, criterion 4: Maintenance of medical devices and equipment
• Standard 5, criterion 5: Medical devices training
| Standard | 1 Governance | 2 Learning from experience | 3 Competant & Capable workforce | 4 Safe Environment | 5 Acute, Community & non NHS providers | 6 MH & LD |
|---|---|---|---|---|---|---|
| Criterion | ||||||
| 1 | Risk management strategy |
Clinical audit | Corporate induction | Secure environment |
Supervision of medical staff in training |
Clinical supervision |
| 2 | Policy on procedural documents |
Incident Reporting | Local Induction of Permanent Staff |
Violence & Aggresion |
Patient Information & Consent |
Patient Information |
| 3 | High Level Risk Committee(s) |
Concerns & Complaints |
Local Induction of Temporary Staff |
Slips,Trips & Falls (Staff & others) |
Consent Training | Clinical Risk Assessment |
| 4 | Risk Management Process |
Claims Management | Risk Management Training |
Slips,Trips & Falls (Patients) |
Maintenance of Medical Devices & Equipment |
Physical Assessment & Examination of Patients |
| 5 | Risk Register | Investigations | Training Needs Analysis |
Moving & Handling |
Medical Devices Training |
Observation of Patients |
| 6 | Dealing with External Recommendations |
Analysis & Improvement |
Risk Awareness Training for Snr. Management |
Hand hygene training |
Screening Procedures |
Dual Diagnosis |
| 7 | Health Records Management |
Learning Lessonsf rom Claims |
Moving & Handling Training |
Innoculation incidents |
Diagnostic Testing Procedures |
Rapid Tranquilisation |
| 8 | Health Record-Keeping Standards |
Best Practice - NICE |
Harassment & Bullying |
The deteriorating patient |
Transfusion | Absent Without Leave (AWOL) |
| 9 | Professional Clinical Registration |
Best Practice - National Confidential Enquiries & Inquiries |
Supporting Staff Involved in an Incident, Complaint or Claim |
Clinical handover of care |
Venous Thromboembolism |
Medicines Management Training |
| 10 | Employment checks |
Being Open | Stress | Discharge | Medicines management |
Medicines management |
NHS Resolution
|
Maintenance of Medical Devices & Equipment |
How does the organisation include all items of diagnostic and therapeutic equipment on an inventory? |
| Medical Devices Training | How does the organisation follows up those who do not complete training? What actions are taken in the event of persistent non-attendance? |
Maintenance of Medical Devices & Equipment
Organisations providing acute and community services and non-NHS providers must have an approved documented process for managing the maintenance of reusable diagnostic and therapeutic equipment.
Level 1
Your documented process must include:
a) Duties
b) How the organisation includes all items of diagnostic and therapeutic equipment on an inventory
c) How reusable diagnostic and therapeutic equipment is maintained
d) How reusable diagnostic and therapeutic equipment is repaired
e) How the organisation monitors compliance with all of the above.
Level 2
You must evidence implementation of your documented process in relation to:
a) How reusable diagnostic and therapeutic equipment is maintained
b) How reusable diagnostic and therapeutic equipment is repaired.
The assessor will review the organisation’s incident database and select two items to assess the organisation’s compliance with the above minimum requirements.
Level 3
You must evidence monitoring of your documented process in relation to:
a) How reusable diagnostic and therapeutic equipment is maintained
b) How reusable diagnostic and therapeutic equipment is repaired.
Where your monitoring has identified shortfalls, you must evidence that changes have been made to address them. The assessor will review the organisation’s incident database and select two items to assess the organisation’s compliance with the above minimum requirements.
Medical Devices Training
Organisations providing acute and community services and non-NHS providers must have an approved document which sets out the training requirements of all permanent staff in relation to the use of diagnostic and therapeutic equipment.
Level 1
Your documented process must include:
a) Duties
b) How the organisation includes all items of diagnostic and therapeutic equipment on an inventory
c) How the organisation identifies which permanent staff are authorised to use the equipment listed on the inventory
d) How the organisation decides the training required
e) How the organisation decides the frequency of updates required
f) How the organisation records that all permanent staff complete training
g) How the organisation follows up those who do not complete training
h) Action to be taken in the event of persistent non-attendance
i) How the organisation monitors compliance with all of the above.
Level 2
You must evidence implementation of your documented process in relation to:
a) How the organisation identifies which permanent staff are authorised to use the equipment listed on the inventory
b) How the organisation decides the training required
c) How the organisation decides the frequency of updates required
d) How the organisation records that all permanent staff complete training.
The assessor will review the organisation’s incident database and select two items to assess the organisation’s compliance with the above minimum requirements.
Level 3
You must evidence monitoring of your documented process in relation to:
a) How the organisation identifies which permanent staff are authorised to use the equipment listed on the inventory
b) How the organisation decides the training required
c) How the organisation decides the frequency of updates required
d) How the organisation records that all permanent staff complete training.
5.5 – Medical Devices Training – incident database to be reviewed by NHS Resolution auditors and two medical devices will be selected.
Sources:
https://assets.publishing.service.gov.uk/media/6089dc938fa8f51b91f3d82f/Managing_medical_devices.pdf
http://www.cqc.org.uk/
https://www.gov.uk/government/publications/managing-medical-devices
Compiled and edited by:
Dr John Sandham CEng FIHEEM MIET