Well, good morning everyone. It’s really strange to see you all! I don’t really know what to say. This is the first live presentation that I’ve given since February 2020, so I’m slightly feeling rusty, so apologies if I seem slightly awkward. Had things all gone to plan last year, I would have been presenting this to you just a few weeks after the launch of two policy reports by the Institution of Mechanical Engineers, of which I was lead author. These reports focus on the future of the engineering workforce and technology adoption in the NHS and are the combined efforts of a number of IMechE members and policy staff with input from experts outside of the institution to ensure that we have reflected the views of our engineering colleagues across the healthcare and med-tech sectors. I am absolutely delighted to be finally getting a chance to revisit these reports ten months after they were first released. So much has obviously happened since then and I am very keen to get your thoughts on whether the situations framed here have changed and what you believe we can do as a community of engineers to generate greater impact across the healthcare sector.
So, let’s get started. Like doctors and other healthcare professionals, chartered professional engineers and technicians have a statement of ethical principles in which we aspire to do no harm by ensuring we do not compromise where society’s welfare and safety is concerned and that we listen and work with society to create transformative technology for the right reasons. It follows then that caring for society forms a fundamental imperative for engineers in healthcare and it is at the forefront of all that we do. Despite incredible progress, healthcare services across the globe will continue to suffer from mounting pressures, driven increasingly by ageing populations with expectations of continuing health and independence into old age, lifestyle conditions, and the impact of poverty in poorer countries. At the same time we are witnessing a rapid expansion in healthcare coverage in developing nations and a medical technology revolution driven by predominantly health data analytics and the digitisation of patient care pathways that are enabling previous intractable conditions to be treated.
Global crises such as the recent pandemic have highlighted that 21st century medicine can only be delivered with significant technology input and that care at home is just as important as care in hospitals. This rapid change in health provision will require comprehensive strategies from government, regulatory authorities and healthcare providers to allow for timely development, evaluation, implementation and regulation of this technology and I know the speakers after me are going to be speaking about those particular subjects as well. In this presentation though, I’m going to focus on two areas highlighted in the reports that the IMechE produced. The first being the value of engineering in healthcare provision, why we need more engineers and the influence that those engineers could have on the healthcare service and the second part is what can the engineering workforce do to address the slow pace of adoption of technology and how might our healthcare providers benefit from their professional understanding of technology in a rapidly changing environment.
Well, before we get to the discussion of these particular points, let’s look first at our healthcare service. Much of the information on these slides is woefully out of date now, I suppose, but you’re all pretty familiar with it and I don’t really need to go into much detail, but we are very proud of our NHS, we recognise that it is one of the most efficient and effective healthcare systems in the world. It’s the biggest employer in the UK and just to put that into perspective, because I know that there’s a few ex-military people here, the British Army only has 125,000 employees, soldiers, and Tata Steel, which is one of the biggest global employers and the biggest engineering firm in the world, has only 80,500 employees. That puts the NHS into perspective. Obviously it sees nearly a million people every 24 hours, and this was a fact that I found amazing and our estates colleagues will be very proud of this, the hospital estates stretches to 25 miles square. It’s the size of Lincoln. That really, really makes me think just how much we do as a profession, yet there are many healthcare systems, it’s the same as any healthcare system across the globe, it is in constant need of improvement and development to ensure it provides the best care to patients, and everybody knows here that takes money, right.
Now, these figures are pre-COVID, but if you think in terms of per person actually the NHS is really good value for money. It’s about £2,500 per adult and if you think that the average wage is about £500 per week it’s really quite a good return on investment, but this cost to taxpayers is only set to increase over the coming years as our population grows and ages and thus treatments for long term illnesses are going to escalate. So, to put that in context, if we compare that to global health, almost half of the world’s healthcare expenditure goes on preventable illnesses such as respiratory and cardiovascular disease, often brought about by lifestyle and environmental conditions of course, and the big one, cancer. On top of this we’re seeing a significant fall in the number of frontline healthcare workers, mainly doctors and nurses particularly in developing countries, but supporting this and all of those wonderful people out there is our med-tech industry. Already it’s getting to the point where it’s surpassing pharma in terms of its size and scale and there are over 500,000 CE marked products available across Europe and most hospitals, as you’re well aware, have tens of thousands of devices in their Trusts, but with the unprecedented swell in healthcare services apps and services across the globe and certainly as a result of COVID, it’s clear that technology is now ubiquitous in everything that we do.
So, with this in mind, what changes can the engineering workforce effect within healthcare, what can we do as a community to ensure that we have greater involvement in the patient care pathway, and the critical question, what will happen if we don’t? Well, COVID, it’s safe to say pre-COVID the existing healthcare engineering workforce had the capability of taking on greater responsibility for technology, innovation and patient care. However, if we continue down a path of greater technological demand, based on new and unchartered disease conditions as well as fewer and fewer engineers available or entering the field with the clinical expertise to design, manufacture and implement technology, we will reach a point where we will be unable to meet patient care need. So, how are we going to address this and really what can engineers do to change that potential direction?
Well, I think you would probably agree it’s often hard to spot an engineer in the NHS, it’s probably even harder to spot a clinical engineer in the NHS, yet we have a community that adds incredible value to patients and we’ve seen that from Ruth’s presentation and from Joe earlier on, the amount of effort by the engineering community that went into just dealing with the Nightingale Hospitals. These engineers, as we all know, they develop devices which diagnose, treat and rehabilitate patients, they create technologies which help measure, model and simulate physiology and anatomy, they’re pioneers of artificial joints and organs and they’ve explored the growing area of digital communication to enable patients to have contact with their doctors 24/7, yet until COVID struck, very few people outside of this room were aware of that.
Now, one of my heroes is Professor Chris Toumazou, who has received over 25 awards for his pioneering advances in DNA sensing and vital signs monitoring. He has been actively developing a new technique for the rapid detection of COVID and his new portable testing device which combines biochemistry, microfluidics, electronic circuits, miniaturisation based on smartphone technology can give a test result in 90 minutes. These are just a few of the hidden faces of our engineering community, both on the frontline and in industry.
So, it’s the IMechE’s view, and certainly the opinion of many I would think in this room, that healthcare engineers should become much more involved in the direct delivery of care to patients and that an appropriately trained workforce is key to ensuring the delivery of safe, affordable care on a global scale and failure to act on these requirements will increase the risk to patients. Healthcare engineers should have, we believe, professional parity with their clinical counterparts. I know this is going to be a revelation for some, particularly within the NHS, but to achieve this the healthcare engineering workforce needs new skills and responsibilities to adapt to the changing healthcare landscape, which would provide a broader end-to-end systems perspective to care, traversing the more vertical specialised expertise of clinical models.
In response to international health challenges the institution has defined a professional commitment for healthcare engineers and this commitment urges all of us to ensure that every hospital has professionally recognised engineers and technicians with consistent qualifications, levels of authority and decision making abilities. To achieve this, the institution defined a professional commitment statement which recognises the healthcare engineers’ commitment to do no harm, but also recognises that healthcare professionals trained in both clinical and technological competencies will be able to safeguard patients through the implementation of quality processes, provide value for money through benchmarking and ensure faster access to medical technology through trialling and product development.
To achieve these goals of recognition we believe that there are two key roles that need to be created. The first is every hospital should have a chief healthcare engineer. These engineers should have levels of authority and decision making responsibilities akin to roles such as head of surgery, chief nurse and chief pharmacist, as well as being part of a national network of chief engineers with connectivity to other hospitals. This would not only promote best practice in procurement, maintenance and use of medical equipment, but increase the opportunity for cost savings across the health service. Now, I recognise that many hospitals have a concept of a chief healthcare engineer and that may already exist where you work, but they are usually under different titles, different departments and levels of authority. The cost of creating this kind of board level post would be recovered from the long term benefits to patients, services, budgets and healthcare providers.
Now, the growing desire to move long term care and treatment out of the clinical setting is creating a new dilemma for already overwhelmed social care services. Steps should be taken to build on the well-proven techniques from rehabilitation and assistive technology engineering to create a patient care pathway at home. Patient enablement engineers and technicians would work exclusively in the space between acute care and social care with their clinical colleagues. They would not only require the full remit of engineering qualifications and skills, but in-depth clinical and social care knowledge, as well as things like management and even customer services experience. Here there is an opportunity then for professional engineering institutions like the IMechE and our sister institutions to work with healthcare providers and with organisations in leadership roles, like the Academy for Healthcare Science, to create new training programmes in areas such as process flow, procurement, purchasing and strategic planning to support engineers working in this area. Now, these two harmonised approaches across healthcare engineering profession would certainly raise the profile and level of importance of engineering in both clinical and med-tech sectors and also aid the recruitment and retention of engineers in our profession.
The new decade is really expected to be nothing short of amazing when it comes to medical devices, we’re all aware of that, but the pace of change is expected to accelerate and it will do now we are moving towards a normal, should I say in inverted commas, way of living and working, but with the increase in multidisciplinary technology entering the sector, including personalised sensing and diagnostics, as well as miniaturisation and greater use of robotics, we all know that the structure of the NHS has yielded significant challenges, shall we say, when it comes to the development and delivery of technology to the frontline. With its mix of centralised authority and regional self-governance, the route to technology adoption within the NHS can be an arduous one and the NHS is often seen as being slightly resistant to innovation which doesn’t deliver an immediate tangible benefit to patients in terms of care or cost saving. This in turn stifles both medium and long term innovation strategies. So, the adoption of technology will be affected even further as this equipment becomes more complex and multidisciplinary with greater interconnectivity, integration, interoperability, and interdependence.
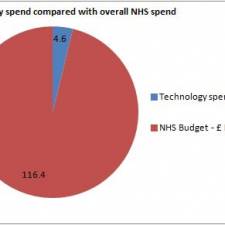
While the digital transformation will address some of the connectivity and data management issues facing UK’s health service, it does fall short in looking at ways to improve medical device and equipment procurement and adoption in the long term, and uptake of technology in the UK has been slow, often due to isolated approaches to procurement and inconsistent distribution of innovation within and between NHS Trusts and these entrenched approaches have often resulted in unsuitable or even poorly specified devices and in some cases technology being incorrectly used or disposed of because it fails to meet the needs of the clinician or the patient. It is likely that if steps are not taken now to create sustainable strategies for complete life cycle technology adoption and greater engagement with the engineering specialists who would oversee it, the NHS may be unable to propagate a coherent and cost effective approach to patient care in the future, but more significantly there remains a mismatch between the money invested in developing technology versus investment to adopt and spread technology at scale and these figures here are from the King’s Fund Report from 2018. The NHS was shown to set aside less than 0.1% per year of available resources for the adoption and spread of innovation compared to the 1.2 billion it was investing in R&D.
Now, according to the World Health Organisation, successful national technology adoption processes often go well beyond patient need and funding and require the engagement of all healthcare stakeholders to deliver successful uptake. The role of GPs, social services, pharmacists and family carers must not be overlooked when we consider how technology is adopted and empowering patients to play a more active role in their own care could drive greater acceptance, compliance and adoption of technology in the long term and here lies, we believe, the opportunity to create a national strategy to address care within the community based on regional need which could yield significant technology uptake and this could be managed through a nationwide network of patient enablement engineers providing patients with access to the right services when they need them.
In order to address the growing demand for more technology, engineers are going to have to be advocates and implement technology at speed and scale that the NHS is comfortable with. Engineers must therefore be empowered to take greater ownership of the procurement and implementation processes for technology across the hospital networks. This would include being directly involved in design, selection, purchasing, maintenance and decommissioning of medical equipment and it was great to hear Joe talking about the decommissioning side as well. So, the institution believes that to deliver safe and affordable care in a fast changing healthcare environment, government and healthcare providers need to be looking to implement national complete life cycle adoption strategies in the medium to long term. This approach would ensure equipment is correctly specified so it would be fit for purpose and deliver the expected patient benefits within budget, as well as being managed sustainably through to its end of life and disposal.
Now, healthcare engineers, we all know, are very well placed to carry out this kind of role, but the benefits of greater involvement and autonomy will only be realised if we have that more consistent approach and coherent approach to their work and skills over time. To achieve this, the IMechE has identified two opportunities which could offer the most widespread engagement with and uptake of technology using complete life cycle approaches. With many countries shifting healthcare focus to prevention rather than cure, greater pressure is going to be placed on our primary care services, as we know. There is an opportunity then to establish a national technology procurement and adoption strategy specifically aimed at GP surgeries to enable more holistic prevention programmes to be supported. Now, we’ve termed these advanced GP surgeries, but I assure you this is not creating another tier of GP surgeries, this is about giving technology to the existing service that we have, but it would contain things like early diagnostics technologies for liver, lung and bowel cancer, for example, as well as rapid blood testing analysis and other preventative technologies. By enabling patients to be tested locally, waiting times and referrals could be reduced to days not weeks and could save thousands, if not millions, of pounds for the long term acute care costs that would have been increased had they had to go into long term care and we also think that remote monitoring, as it’s becoming increasingly important for managing the impact of conditions like obesity and diabetes, age conditions like Alzheimer’s and frailty, as well as end of life palliative care, effective management and support of remote monitoring systems and home diagnostic appliances in social care settings will need people who are both trained technically and clinically to enable them to manage these pieces of equipment.
A remote health monitoring network that integrates acute and social care using data analytics, wearables, sensors, could really, really make a difference to the provision of easing logistical pressures on our existing healthcare service and a key way that we could standardise our remote healthcare monitoring equipment would be to enable patients to be informed about their illnesses wherever they are in the country. Wouldn’t that be a lovely thing? With the constant turnover of monitoring equipment, and Joe alluded to that as well, a complete life cycle technology adoption strategy would really ensure that patients have access to and benefit from the right technologies and that they’re fit for purpose and tailored to their needs.
So, that is a bit of a whistle-stop tour through, thank you John, but just to conclude, the Institution of Mechanical Engineers is really committed to ensuring that performance, safety and ethical standards are maintained across the profession when it comes to creating transformative technologies such as the stuff that we see out there today and the IMechE feels it is well-placed, along with its sister institutions, we do not work alone in this, to support healthcare engineers in providing workable and cost effective solutions that will inform decision making at all levels of government and care provision. In ever more technical surroundings we need engineers to ensure our healthcare providers are able to make the best decisions possible regarding medical equipment and technology which can facilitate early diagnosis and provide better and more effective treatments to patients. In response to international healthcare challenges, the institution urges all healthcare engineers across the globe to continue to establish, strengthen and share strategies and best practice processes for life cycle technology adoption through formal engineering communities and networks such as what we’re here today for, John.
Innovation cannot be expected to spread passively. To ensure active acceptance by patients and practitioners, it requires insight into the application, awareness of the clinical setting and an in-depth knowledge of the devices’ function. The realistic and long term adoption of technology can no longer be the sole responsibility of the clinician but must include healthcare engineers who are able to implement innovations and adapt them to the local environments ensuring a safe passage for our patients through our healthcare system
Thank you very much.
Dr. Helen Meese's presentation at the EBME Expo Reforming Clinical Engineering